Comparing adult height gain and menarcheal age between girls with central precocious puberty treated with gonadotropin-releasing hormone agonist alone and those treated with combined growth hormone therapy
Article information
Abstract
Purpose
This study aimed to investigate the outcomes of gonadotropin-releasing hormone agonist (GnRHa) therapy with or without growth hormone (GH) therapy for girls with idiopathic central precocious puberty (CPP).
Methods
The medical records of 166 girls diagnosed with CPP from 2002 to 2017 were retrospectively reviewed. All included patients were treated with GnRHa for ≥36 months. Changes in height standard deviation score (SDS) for bone age, chronological age (CA), and predicted adult height (PAH) were assessed for the first three years of treatment. The final height gain SDS was calculated as the difference between the initial PAH SDS and adult height (AH) SDS; these were then compared between the GnRHa group (group A, n=135) and the combined GnRHa/GH group (group B, n=31).
Results
The initial mean CA was 7.89 years. The mean menarcheal age was 13.12 years (group A, 13.1±0.99; group B, 13.18±0.58 years; P=0.755). PAH SDS at the start of GnRHa treatment and AH SDS were significantly lower in group B than in group A (PAH SDS: -2.20±0.83 vs. -3.19±0.84, P<0.001; AH SDS: 0.18±084 vs. -0.30±0.66, P=0.021). The increase in PAH SDS was higher in group B than in group A for the first three years of GnRHa treatment (1.66±0.66 vs. 2.35±0.93, P<0.001). The height gain SDS was significantly higher in group B than in group A (2.5±0.75 vs. 2.93±1.02, P=0.048). Younger age, higher PAH at the start of treatment, and a greater increase in PAH SDS during the first year of GnRHa treatment positively affected AH.
Conclusions
The combined GH group had more additional height gain than the GnRHa-alone group.
Introduction
Patients with precocious puberty (PP) develop pubertal sex characteristics due to early activation of the hypothalamic-pituitary-gonadal (HPG) axis before the age of 8 years in girls and 9 years in boys. Premature pulsatile secretion of gonadotropin-releasing hormone (GnRH) leads to the release of luteinizing hormone (LH) and follicle-stimulating hormone, and these hormones subsequently stimulate the synthesis and secretion of estradiol (E2). This results in increased serum insulin-like growth factor-1 (IGF-1) levels [1,2]. This series of hormonal changes accelerates the maturation of bones, which may lead to a shorter height when the patient is an adult. The incidence of PP has been reported to be approximately 1:5000–1:10,000, and it is 10 times more common in girls than in boys [3]. In most cases the abnormal functioning of the HPG axis is idiopathic, although in rare cases intrasellar neoplasm, hematoma, hydrocephalus, brain injury, or hypothyroidism can be the cause [4,5]. These are often termed "true" and "pseudo" PP, respectively, or central PP (CPP) and peripheral PP, respectively [6].
To prevent potential social maladjustment of the patients, it is necessary to minimize the early development of sexual characteristics and height loss. Thus, the use of GnRH agonists (GnRHas) has been a common treatment for CPP for more than 30 years since the use of leuprolide acetate was reported in 1981 [7] and 1989 [8]. Administration of GnRHas interferes with the pituitary-gonadal axis and reduces E2 release from the ovaries [9]. It also leads to reduced growth velocity (GV), inhibited bone growth, and suspended or decreased development of secondary sex characteristics [5]. Consequently, GnRHa treatment is helpful in postponing pubertal development and retaining height potential. Several studies have demonstrated the efficacy of GnRHa treatment including improved final adult height (AH), especially in patients younger than 6 years of age [6,10-15]. However, other studies have reported that GnRHa treatment decreases active IGF-1s levels leading to relatively small gain in AH [16-18]. In these cases, it would be reasonable to compensate for the reduction in IGF-1 levels during GnRHa therapy by combining growth hormone (GH) with the GnRHa treatment [19-21].
The aim of this study was to compare the final outcomes of patients treated with GnRHa therapy with and without combined GH treatment. This included detailed evaluations performed during the three years after the initiation of GnRHa treatment and an investigation of factors that could have affected stature outcome.
Materials and methods
1. Subjects
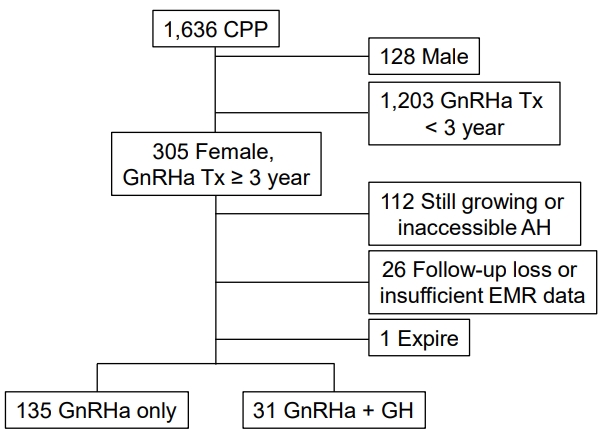
We performed retrospective reviews of medical records from the Pediatric Department of Bundang Jesaeng General Hospital, Daejin Medical Center, Korea, from January 2002 to December 2016. Of the 1,636 patients who were diagnosed with CPP, 166 girls with CPP who were treated with GnRHa for ≥36 months were selected. The patients were divided into 2 groups: those who received GnRHa alone (group A, n=135) and those who received GnRHa combined with GH (group B, n=31) (Fig. 1). AH and menarche data were available for 86 subjects. Thus, all statistics, including AH and menarche, were performed with 86 subjects (group A, n=66). The classical diagnostic criteria for idiopathic CPP were an age of 8 years or less at breast development (i.e., Tanner stage B2 or above), bone age (BA) advancement (i.e., at least 1 year more than chronological age [CA]), a peak LH level determined with electrochemiluminescence immunoassays above 5 IU/L during a standard GnRH-stimulation test, and no evidence of organic lesions on the hypothalamic-pituitary axis confirmed using magnetic resonance imaging scans. Patients who had other conditions, such as thyroid disease, genetic impairment, and ovarian or adrenal diseases, were excluded. Patients who had abnormal androgen release and congenital adrenal hypertrophy were also excluded from the analysis of serum 17-hydroxyprogesterone and delta 4-dehydioepiadrostendione sulfate levels. GH was given to patient who either fell below the fifth percentile for predicted adult height (PAH) at the time of diagnosis, fell below the fifth percentile for midparental height (MPH), or had a slow GV of under 5 cm per year.
2. Methods
All patients were administered GnRHa at a dose of 60–90 μg/kg every 4 weeks. In group B, patients were additionally treated with GH at a dose of 0.25 mg/kg every week. Height, weight, and pubertal advancements were recorded for all patients every 4 weeks after the first visit. The BA was recorded every 6 months. Data collected at the beginning of the GnRHa treatment, at 1, 2, and 3 years after the initial treatment, and at the end of GnRHa treatment was used in this analysis. Height was measured to the nearest 0.1 cm using a Harpenden Stadiometer (Holtain Ltd., Crymych. UK). BA was assessed using the Greulich-Pyle method [22] by the same observer using anteroposterior view films of the left wrist. MPH was defined as the average of the parental heights minus 6.5 cm. PAH was calculated using the average Bayley-Pinneau method [23]. Annual changes in height were assessed and expressed as a standard deviation score (SDS) for CA and BA using the 2017 Korean National Growth Charts [24]. PAH, MPH and AH were also expressed as SDSs for the purpose of comparing them. We made inquiries regarding AH for patients who had grown less than 1 cm a year, were at least 2 years past their menarcheal age, and who had a BA over 15 years. AH was collected via telephone interviews, and height and BA were confirmed in the outpatient clinics. The menarcheal age of these 86 girls was also reported by patients. To demonstrate the effectiveness of the treatment, we evaluated the differences between the SDSs for AH and initial PAH, for AH and MPH, and for AH and initial height.
Blood chemistry parameters, such as thyroid stimulating hormone, free thyroxine, E2, total estrogen, LH, IGF-1, and IGF-binding protein 3 (IGF-BP3), were measured using a Hitachi Automatic Immunology Analyzer (Cobas E170, Roche, Rotkreuz, Switzerland) at the initial diagnosis and the end of the GnRHa treatment.
3. Statistical analysis
The IBM SPSS Statistics ver. 24.0 (IBM Co., Armonk, NY, USA) was used for the statistical analyses of the data. All data are expressed as the mean±standard deviation. The paired t-test was applied to compare data within each group, and the independent t-test was used to make comparisons between the 2 groups. Multiple linear regression analysis was used to determine correlations between multiple parameters and height outcome. A P-value of <0.05 was considered statistically significant.
Results
1. Characteristics and auxological data
The mean CA and BA of patients at the beginning of GnRHa treatment were 7.89±0.81 and 9.67±0.91 years, respectively. The BA was 1.78±0.70 years more than the CA at the start of GnRHa treatment. All patients were treated with GnRHa for 45.25±8.45 months. Patients in group B were treated for longer than those in group A (P=0.017). The mean duration of GH treatment was 39.23±16.94 months. After the initiation of GnRHa treatment, it was a mean of 19.19 months before GH treatment was started. The initial height of patients was 128.17±0.7 cm, and the PAH was 149.96±4.03 cm. The patients in group B had a lower initial height and PAH (P<0.001 for both). The height at the end of the treatment was 148.99±4.27 cm and 148.62±3.67 cm for groups A and B, respectively; however, this was not significantly different. The BA, ΔBA-CA, and PAH were significantly different between groups A and B at the start of the treatment, but there was no statistically significant differences between the 2 groups at the end of GnRHa treatment. The MPH, as the target height, and the AH of the patients in group A were higher than in group B (MPH; P<0.001, AH; P=0.02). The mean menarcheal age was 13.12 years. The time between menarche and the end date of GnRHa therapy was not statistically significantly different between the 2 groups (Table 1). There were no statistically significant differences between the 2 groups for other biochemical laboratory tests, including IGF-1 and IGF-BP3, at start of GnRHa treatment (Table 2).
2. Comparison of growth outcomes during first three years of GnRHa treatment
The increase in PAH SDS from the beginning of GnRHa treatment to the third year (ΔPAH SDS 0–3) was significantly higher in group B than in group A (P<0.001). The increase in height SDS for BA (SDSb) and CA (SDSc) from the start to the third year of GnRHa treatment were also statistically higher in group B (P<0.001 for both) (Table 1; Figs. 2, 3). The PAH SDS, height SDSb, and height SDSc significantly increased at the end of GnRHa treatment (P<0.001 for all), and the increases were greater in group B (P<0.001 for all).

Changes in height SDSc (A), height SDSb (B), PAH (C), and PAH SDS (D) of subjects with CPP by type of treatment (black, group A; grey, group B). Group A, GnRHa alone group; group B, combined GnRHa/GH group; SDS, standard deviation score; SDSc, standard deviation score for chronological age; SDSb, standard deviation score for bone age; GnRHa, gonadotropin-releasing hormone agonist; PAH, predicted adult height; Tx, treatment. *P<0.05 vs. 1 year ago. ***P<0.001 vs. 1 year ago.
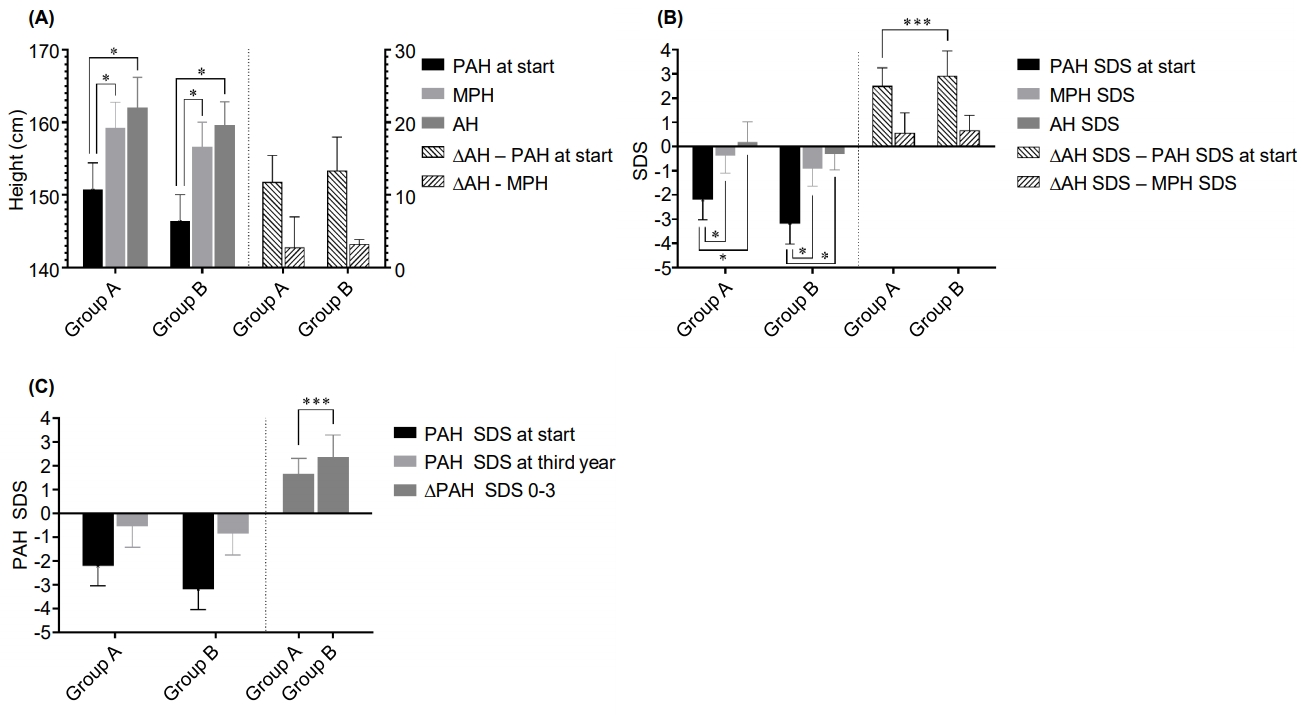
Comparison of PAH, MPH, AH, and changes in subjects with central precocious puberty by type of treatment, expressed as (A) height, (B) SDS, and (C) PAH SDS for the first 3 years of gonadotropin-releasing hormone agonist (GnRHa) treatment. Group A, GnRHa alone group; group B, combined GnRHa/GH group; PAH, predicted adult height; MPH, midparental height; AH, adult height; SDS, standard deviation score. *P<0.001 vs. PAH or PAH SDS at start of GnRHa treatment. ***P<0.001 between the GnRHa group and the GnRHa plus GH group.
3. Comparison of AH growth outcome
In terms of therapeutic effects, the AH (161.47±4.10 cm) was over the target height (158.75±3.63 cm) and significantly higher than the initial PAH in each group (P<0.001). The AH SDS was also significantly greater than the initial PAH SDS and MPH SDS in each group (P<0.001) (Fig. 3). The height gain (ΔHG), which is the difference between the AH SDS and the initial PAH SDS, was significantly higher in group B, although the difference between AH and initial PAH was not statistically significant (Table 1). Also, HG calculated as the difference between AH SDS and initial height SDSb was not significantly different between the 2 groups.
4. Correlation between AH and other auxological factors
Multiple regression analysis was used to identify factors influencing AH (Table 3). Only the patients from group A were used in this analysis; those in group B were excluded because GH treatment could be a confounding factor. A younger initial CA, a higher initial PAH SDS, and a greater increase in PAH SDS 1 year after the start of GnRHa treatment were significantly positively correlated with AH (Table 1, Fig. 2). The BA at the start of treatment, MPH SDS, and the duration of the GnRHa treatment did not correlate with AH.
5. Menarcheal age
Menarche occurred at 13.12±0.92 years of age, and there were no statistically significant differences between the 2 groups (P=0.775) (Table 1). The duration from the end of GnRHa treatment to menarche was 17.80±8.02 months, but there was no significant difference observed between the groups (P=0.075).
Discussion
We performed a retrospective review of 166 patients with CPP who were treated with GnRHa either in combination with GH or without for more than 3 years and evaluated the long-term effects.
For the first 3 years overall of GnRHa treatment, the increase in PAH SDS was significantly higher in group B. However, the annual increase in PAH SDS was higher in group B than in group A for each of the first 2 years, but there was not a clear difference in the third year (first year, P=0.02; second year, P=0.008; and third year, P=0.108) (Fig. 2). The AH SDS was significantly higher than the PAH SDS at the start of GnRHa treatment in both groups. The increase in height gain in group B was 2.93 SDS, which was a greater increase compared to group A (approximately 2.5 SDS). In addition, a younger CA, higher PAH SDS, and greater increase in PAH SDS in the first year were correlated to a greater increase in AH.
In 1991, Oostdijk et al. [25] reported that combined GnRHa/GH treatment improved PAH in three girls with CPP who had a low GV when treated with GnRHa alone. Subsequent studies have also described better outcomes for girls treated with combination therapy [20,26-30], and some Korean reports have also been published [31,32]. Volta et al. [33] highlighted that the combined treatment could be helpful for CPP patients with slow growth. Jung et al. [31] found a greater difference between AH and PAH at the beginning of treatment in the GnRHa plus GH group compared to the GnRHa-alone group, but this was not a significant statistical difference. Gyon et al. [32] reported that the combined treatment group had a significantly higher increase in height from PAH at the start to near final height (NFH) (P<0.001). These results are similar to the present report. Those 2 Korean studies also evaluated factors that positively influence AH SDS and NFH. In the study of Jung et al. [31], younger CA and taller MPH were factors, and in the study of Gyon et al. [32], taller height at the start, taller MPH, and longer treatment duration were factors. These previous results are partially in line with present study. The menarcheal age in this study was 13.12±0.92 years and older than the study of Gyon et al. [32] at 11.6±0.8 years. The time from the end of GnRHa treatment to menarche was 17.80±8.02 months in this study, which was longer than the 15.7±6.4 months in Gyon et al. [32] or the 1.0±0.61 years in Jung et al. [31] This could be the result of the inclusion criteria for this study of GnRHa treatment of 36 months or more.
To our knowledge, our study is the largest retrospective, single-center study that compared statural outcomes in girls with CPP after treatment with GnRHa alone or GnRHa plus GH. In addition, our study was strictly controlled for more than three years of GnRHa treatment for all patients.
The limitations of our study are as follows: (1) PAH SDS, height SDS, and MPH SDS at the start of treatment were significantly lower in the GnRHa plus GH group. This indicates that the subjects were not sufficiently randomized for both therapies, possibly due to a selection bias. (2) The results might be influenced by the differences in the duration of GnRHa treatment. Furthermore, in the GnRHa plus GH group, it is difficult to determine whether the higher ΔHG was due to the addition of GH or the longer duration of GnRHa therapy. Thus, we compared the change of PAH SDS for the first 3 years of GnRHa treatment between the two groups, which indicated that additional GH administration caused the greater increase in HG. (3) In our study, there was a statistically significant difference between the 2 groups for ΔHG (P=0.048), but AHPAH at the start was not significantly different (P=0.124) (Table 1). This is relatively weak evidence compared with the previous report by Gyon et al. [32] (P<0.001). (4) We used the Bayley-Pinneau method with average tables to estimate PAH at the start of GnRHa treatment, which can relatively underestimate PAH compared with the other table, thus affecting the presented height gain. (5) We used the 2017 Korean National Growth Chart as a reference. However, some of the subjects were treated according to the 2007 Korean National Growth Chart or the growth standard index available at the time of treatment, which might be different from the SDS value considered for treatment and the SDS value shown in this study. However, the 2017 growth standard index was used consistently in this study; therefore, the comparisons between the subjects are believed to be reliable. However, more rigorous randomized controlled studies will be needed in the future.
In conclusion, GnRHa treatment increased adult height in girls with CPP, and GnRHa plus GH therapy can lead to a greater final height than GnRHa-alone therapy. Also, the increase in PAH SDS during the first year of GnRHa treatment can be a predictive tool to estimate therapy effectiveness.
Notes
Ethical statement This study was approved by the Institutional Review Board (IRB) of Bundang Jesaeng General Hospital (IRB No. PD18-01), and an exemption was made for the requirement of informed consent.
Conflict of interest No potential conflict of interest relevant to this article was reported.