Development of delayed thyroid stimulating hormone elevation in small-for-gestational-age infants: is a second screening needed?
Article information
Abstract
Purpose
Recent reports indicate that small for gestational age (SGA) could be a risk factor for delayed thyroid stimulating hormone (dTSH) elevation in preterm infants. The development of dTSH elevation in SGA late-preterm infants with a gestational age of 34–36 weeks has been investigated in only a few studies.
Methods
In the present retrospective study, 70 SGA infants and 86 sex- and gestational age-matched controls who presented with normal results on initial thyroid function testing were included.
Results
SGA infants had a significantly higher prevalence of dTSH elevation (15.7% vs. 3.5%, P=0.009) compared with appropriate-for-gestational age infants. In SGA infants, the mean age at the time of dTSH was 24 days. Development of dTSH was associated with SGA and medical treatment with dopamine or furosemide. After adjusting for confounding factors, multiple logistic regression analysis showed SGA was a significant risk factor for the development of dTSH elevation (odds ratio, 23.2; 95% confidence interval, 2.27–236.91; P=0.008).
Conclusions
SGA infants may be at risk for dTSH and clinicians could consider a second thyroid screening test around the age of 1 month.
Highlights
· SGA infants with a gestational age of 34–36 weeks may be at the risk of development of delayed TSH elevation and clinicians may consider performing a second thyroid screening test in these infants at 1 month of age.
Introduction
Thyroid hormones play an important role in growth and neurocognitive development. Neonatal screening enables early identification and treatment of congenital hypothyroidism, thereby improving long-term outcomes. The need for a second screening has recently been suggested because extremely-low-birth-weight and very-low-birth-weight (VLBW) infants have a higher incidence of congenital hypothyroidism with delayed thyroid stimulating hormone (dTSH) elevation than infants weighing ≥1,500 g [1]. Considering the possibility of a missed diagnosis on initial screening, the European Society for Paediatric Endocrinology recommended a second screening in preterm neonates, low-birth-weight and VLBW neonates, neonates admitted to the neonatal intensive care unit (NICU), neonates who were tested within the first 24 hours of life, and infants from multiple pregnancies particularly same-sex twins [2]. The mechanism how dTSH develops in these infants is not clearly understood. Possible mechanisms include an attenuated hypothalamic-pituitary-thyroid response, exposure to medication, and a clinical condition that requires NICU admission [3].
In recent studies, small for gestational age (SGA) was reported a potential risk factor for the development of dTSH in preterm infants [4,5]. However, the development of dTSH in SGA infants with a gestational age of 34–36 weeks has been investigated in only a few studies. Therefore, the prevalence of dTSH in late-preterm infants who were SGA was examined in the present study, and the requirement for a second thyroid screening in these infants was determined.
Materials and methods
1. Study design and participants
This single-center retrospective study was performed to compare the prevalence of dTSH between SGA and appropriate-for-gestational-age (AGA) infants born at Keimyung University Dongsan Medical Center between January 1, 2015 and December 31, 2019. SGA infants with a gestational age of 34–36 weeks who had a normal result on the first neonatal screening test for congenital hypothyroidism and underwent at least one follow-up test were included in the study. Neonatal screening was performed between the ages of 48 hours and 8 days. SGA was defined as a birth weight <10th percentile for a given gestational age and sex per the reference values for Korean infants [6]. Gestational age was estimated based on the mother's last menstrual period and ultrasonography findings. Nursing staff used a portable electronic device to measure the birth weight of the patients after the infants were undressed. Infants with maternal autoimmune thyroid disease, multiple congenital malformations, inborn errors of metabolism, and kidney failure were excluded. The control group consisted of sex- and gestational-age-matched AGA infants who underwent a second thyroid screening test after having a normal result on the first thyroid screening test. The following infants were excluded: gestational age <34 weeks or >37 weeks, large-for-gestational-age (LGA) infants whose birth weight was >90th percentile for a given gestational age [6], infants who showed abnormal results on the first thyroid screening test, or if a second screening test was not performed. During the study period, 2,335 infants were born at our hospital with a gestational age ≥34 weeks and <37 weeks. Among the 2,335 infants, 351 infants were SGA, 1,833 infants were AGA, and 151 infants were LGA. Among 351 SGA infants and 1,833 AGA infants, 228 SGA and 1,646 AGA infants who did not undergo a second screening test were excluded. After excluding patients who showed abnormal results on the first thyroid screening test or who underwent a second screening test at the age of <48 hours or 8 days, the final cohort included 70 SGA infants (SGA group) and 86 AGA infants (AGA group).
2. Definitions
The reference range of TSH varies between studies, thus, we defined dTSH as an elevation ≥10 mU/L at the second screening test after a normal result was obtained at the first screening test [7-9]. A patient with a TSH level ≥10 mU/L at the third screening test whose second TSH level was ≥5 mU/L and <10 mU/L and a normal result at the first screening test was also considered as having dTSH. A free tetraiodothyronine (FT4) level<0.9 ng/dL was considered abnormal. Levothyroxine (LT4) treatment was initiated if the venous TSH level was >20 mU/L per the European Society for Pediatric Endocrinology consensus guidelines [2]. If the venous TSH level was 6–20 mU/L, LT4 treatment was initiated after discussion with the parents.
3. Screening protocol
The first thyroid screening test was performed between 48 hours and 8 days after birth. The TSH level was measured in blood samples obtained via heel prick and eluted from filter paper using a dissociated enhanced fluoroimmunoassay kit. Biochemical testing for TSH was performed using the Perkin Elmer AutoDELFIA immunoassay system. Venous TSH level testing was considered the first thyroid screening test in control infants who underwent this test before the filter paper test.
Blood sampling for the second screening test was performed using venipuncture. TSH and FT4 levels were measured using a Cobas 8000 e 801 analyzer (electrochemiluminescence, Roche, Diagnostics, Basel, Switzerland) according to standard protocols. If the TSH level was ≥5 mU/L, further thyroid function testing was performed until the TSH level was <5 mU/L in a venous blood sample.
4. Data collection
The electronic medical records of the infants were reviewed and data associated with the following factors that may affect thyroid function were collected: maternal pregnancy-induced hypertension or gestational diabetes mellitus, cesarean section, multiple gestation, gestational age, birth weight, sex, Apgar score, respiratory distress syndrome, need for respiratory support, necrotizing enterocolitis, congenital heart disease, and history of exposure to medications such as antenatal steroids, vancomycin, furosemide, or dopamine.
5. Statistical analyses
Statistical analyses were performed using the IBM SPSS Statistics ver. 20.0 (IBM Co., Armonk, NY, USA). The Student t-test or Mann-Whitney U-test were used to compare continuous numerical data between the 2 independent study groups depending on the normality of the data distribution. The chi-squared test or Fisher exact test were used to compare categorical data between study groups. The factors associated with a significant odds ratio for dTSH were determined using multiple logistic regression analysis. Factors significant in the univariable regression analysis and associated with dTSH were selected as potential confounding factors in the logistic regression analysis. A P-value of <0.05 was considered statistically significant.
6. Ethical statement
The Institutional Review Board (IRB) of the Keimyung University Dongsan Hospital approved this study (IRB No. 2020-02-055) and a waiver for documentation of consent was approved.
Results
1. Clinical characteristics of the patients and controls
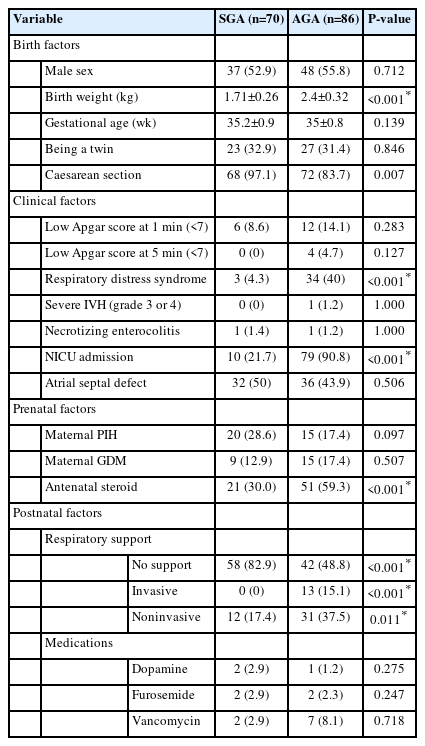
Table 1 shows the clinical characteristics of SGA infants (n=70) and AGA infants (n=86). Based on the inclusion criteria, gestational age did not significantly differ between SGA infants and AGA infants. The birth factor including sex distribution and twin status did not significantly differ between the SGA and AGA groups. Births via cesarean section were significantly more prevalent in SGA infants. Among twins, 4 twins (eight patients) born from 4 mothers were included in the SGA group. Among the 3 sets of twins (6 patients) born from 3 mothers, 3 were SGA and 3 were AGA infants. SGA infants had a significantly lower birth weight (1.71 kg) compared with AGA infants (2.4 kg, P<0.001). Regarding clinical factors, the prevalence of low Apgar scores (<7) at 1 minute and 5 minutes, severe intraventricular hemorrhage, necrotizing enterocolitis, and atrial septal defects were not significantly different between SGA and AGA infants. However, respiratory distress syndrome (4.3% vs. 40%, P<0.001) and NICU admission (31.4% vs. 90.7%, P<0.001) were significantly less prevalent in SGA infants compared with AGA infants. Prenatal factors including maternal pregnancy-induced hypertension and gestational diabetes mellitus did not significantly differ between the SGA and AGA groups. However, antenatal steroid exposure was significantly more prevalent in AGA infants compared with SGA infants. In terms of postnatal factors, the use of invasive or noninvasive respiratory support was significantly lower in SGA infants (17.4%) than in AGA infants (48.8%) (P<0.001). Exposure history to dopamine, furosemide, or vancomycin did not significantly differ between the SGA and AGA groups.
2. Thyroid function test results
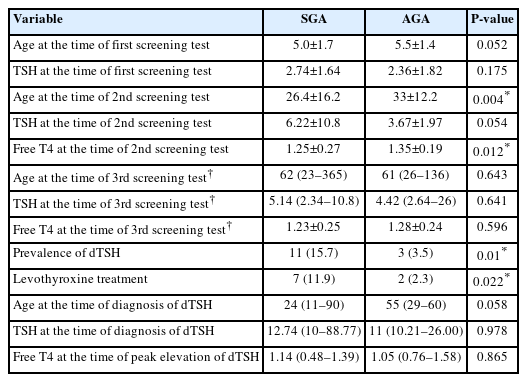
Table 2 shows the thyroid screening test results of SGA and AGA infants. The mean age of the SGA infants and AGA infants at the time of the first neonatal screening was 5 days and 5.5 days, respectively (P=0.052). Mean TSH levels at the time of the first screening test of the SGA and AGA infant groups were 2.74 mU/L and 2.36 mU/L, respectively (P=0.175). All the SGA infants and AGA infants underwent a second screening test at a mean age of 26.4 days and 33 days, respectively (P=0.004). Mean TSH level was marginally higher in SGA infants (6.22 mU/L) than in AGA infants (3.67 mU/L) (P=0.054), and FT4 levels were significantly lower in SGA infants (1.25 ng/dL) than in AGA infants (1.35 ng/dL) (P=0.012).
Due to the retrospective study design, total bilirubin levels were available for a subset of the SGA infants (n=24) and AGA infants (n=59). Total bilirubin levels were not significantly different between SGA infants (3.9 mg/dL) and AGA infants (3.7 mg/dL) (P=0.718). At the second screening test, 10 SGA infants and 1 AGA infant had a venous TSH level >10 mU/L. A third thyroid function test was performed in a subset of SGA infants (n=17) and AGA infants (n=20) with TSH levels >5 mU/L at a median age of 62 days and 61 days, respectively (P=0.643). Only 1 SGA infant with a previous venous TSH level of 5–10 mU/L was newly diagnosed with dTSH. Two AGA infants with a previous TSH level of 5–10 mU/L were newly diagnosed with dTSH. At the third thyroid function screening test, TSH and FT4 levels were not significantly different between the SGA and AGA groups.
The SGA infants had a significantly higher prevalence of dTSH (15.7%) than AGA infants (3.5%) (P=0.01). Among the twins (one SGA and the other AGA), no subject was diagnosed with dTSH. The median age at the time of dTSH diagnosis in SGA infants and AGA infants was 24 days and 55 days, respectively (P=0.058). TSH levels at the time of dTSH did not significantly differ between SGA (12.74 mU/L) and AGA infants (11.0 mU/L) (P=0.978). FT4 level at the time of dTSH also did not significantly differ between SGA infants (1.14 ng/dL) and AGA infants (1.05 ng/dL) (P=0.865).
3. Risk factors for the development of dTSH in SGA and AGA infants
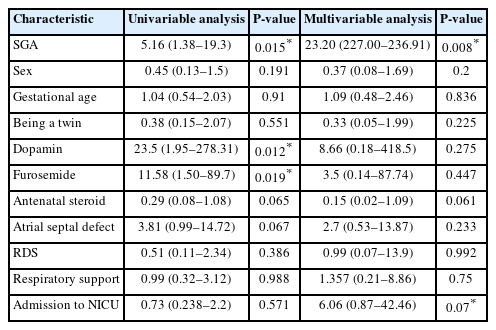
Table 3 presents the logistic regression analyses results. In univariable analysis, infants with dTSH (odds ratio, 5.16; 95% confidence interval, 1.38–19.3; P=0.015) were more likely to be SGA. Dopamine (odds ratio, 23.5; 95% confidence interval; 1.95–278.31; P=0.012) and furosemide (odds ratio, 11.58; 95% confidence interval, 1.5–89.7; P=0.019) were associated with dTSH. In multiple logistic regression analysis, SGA was the only significant risk factor for the development of dTSH (odds ratio, 23.2; 95% confidence interval, 2.27–236.91; P=0.008) after adjusting for sex, gestational age, admission history to NICU, being a twin, application of a ventilator, atrial septal defect, respiratory distress syndrome, and medical treatment with steroid, dopamine, or furosemide.
4. Clinical characteristics of the SGA infants who received LT4
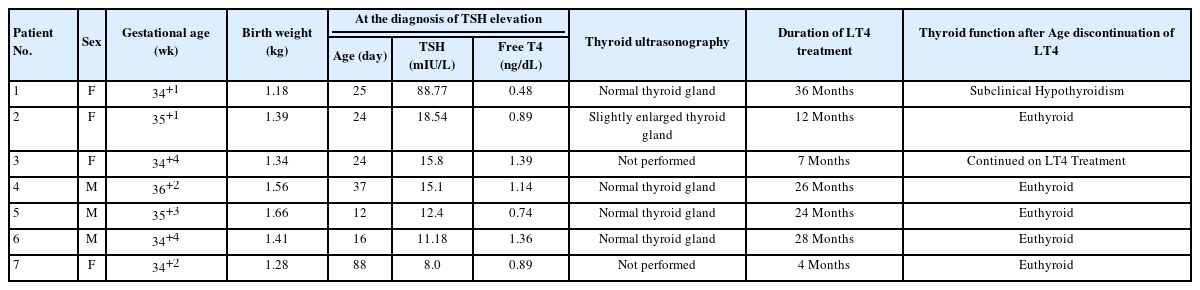
Table 4 shows the clinical characteristics of the 7 SGA infants who received LT4 due to elevated TSH. Three of the SGA infants were male and 4 were female. The highest TSH level (88.77 mU/L) was observed in patient 1 at the age of 25 days. Patients 2, 3, 4, and 6 with TSH levels between 10–20 mU/L were started on LT4 therapy after a discussion with their parents. Patients 5 and 7 received LT4 due to a low FT4 level. Treatment was initiated before the age of 1 month except for patients 4 and 7. Transthoracic echocardiography was performed in 6 patients (except for patient 5) and atrial septal defects were present in all 6 patients. Thyroid ultrasonography was performed in 5 patients (except for patients 3 and 7). Patient 1 with a TSH level of 88.77 mU/L had a slightly enlarged thyroid gland, which might be associated with thyroid dyshormonogenesis. Patients 1, 2, 4, 5, 6, and 7 underwent re-evaluation after the discontinuation of LT4 therapy. Patient 3 has continued LT4 treatment for 7 months to the time of study. Duration of LT4 treatment was between 4 months and 36 months. None of the 6 patients required further LT4 therapy.
Discussion
In the present study, SGA was a risk factor for the development of dTSH in infants with a gestational age of 34–36 weeks. The development of thyroid dysfunction in SGA infants has been previously studied. Uchiyama et al. reported SGA was a risk factor for the development of dTSH in infants with a birth weight<2,000 g and mean gestational age of 27.4 weeks [5]. The development of dTSH occurred at a median age of 37 days. In a Korean study including NICU-admitted VLBW infants with mean gestational age of 28 weeks, SGA was more prevalent in the group treated with LT4 [10]. Liu et al. [4] compared infants with a gestational age <28 weeks with early- to mild-preterm infants (gestational age 28–36 weeks) admitted to the NICU and found that SGA preterm infants had a significantly higher TSH level (3.74 mU/L vs. 3.01 mU/L, P<0.018) and a higher incidence of transient hypothyroxinemia with delayed hyperthyrotropinemia than AGA infants.
The etiology of dTSH in SGA infants has not yet been fully elucidated. In preterm infants, especially those with a gestational age <30 weeks, immaturity of the hypothalamic-pituitary-thyroid axis may contribute to the development of dTSH [11]. Lower birth weight has also been associated with dTSH [12]. Congenital heart disease, the use of medications such as insulin, furosemide, and vancomycin, and exposure to iodine have also been identified as risk factors for the development of dTSH [13].
In contrast to previous studies, late-preterm infants with a gestational age of between 34–36 weeks were included in the present study to reduce the effect of prematurity, which is an independent risk factor for dTSH. Indicators of clinical severity associated with the development of dTSH, including respiratory distress syndrome, application of ventilator, and NICU admission were less prevalent in SGA infants. Being a twin, lower Apgar scores, atrial septal defects, and postnatal medication exposure were equally prevalent in the dTSH infants compared with the non-dTSH infants. Despite the small number of risk factors described above, the prevalence of dTSH was significantly higher in SGA infants than in AGA infants. Among the factors associated with thyroid function, antenatal steroid use was possibly associated with lower TSH levels in preterm infants due to the effect of cortisol on the maturation of the hypothalamus-pituitary-thyroid axis [14]. In the present study, antenatal steroid was more prevalent in AGA infants than in SGA infants. However, the reason for discrepancy could not be explained and further research is needed.
SGA may affect thyroid function. In the present study, the TSH level at the second screening test was marginally higher in SGA infants than in AGA infants. In a study including 5,918 preterm infants (gestational age<37 weeks), significantly higher TSH levels were observed in SGA infants than in AGA infants. In addition, TSH levels increased as intrauterine growth retardation increased [15]. In a study including 14,092 newborns, SGA term infants had significantly higher TSH levels than AGA term infants [16]. In another study, the TSH standard deviation scores of 125 short SGA children (>8 years of age) were significantly higher than the reference values, with TSH levels above the normal range in 3 subjects [17].
Considerable controversy exists regarding the neurodevelopmental outcomes of hyperthyrotropinemia. In term infants, transient hyperthyrotropinemia, defined as TSH elevation after 48 hours of life that resolved after 2 weeks, was associated with persistent hyperthyrotropinemia and developmental delay at 6 years of age [18]. Furthermore, persistently elevated TSH level >5 mU/L after 3 months was associated with impaired neurological outcomes at 18 months of corrected age [19]. However, data regarding long-term neurodevelopmental outcomes are lacking.
When considering the cases where LT4 treatment was initiated, only one patient had a TSH level >20 mU/L, and the other infants treated with LT4 had a TSH level of 10–20 mU/L. When TSH values are at the levels described above, deciding whether to administer LT4 is difficult for clinicians. Because there were no cases of permanent hypothyroidism, even if TSH is elevated, delaying LT4 treatment could be beneficial.
The present study had a few limitations. First, the number of SGA infants included was insufficient to draw definitive conclusions. Second, due to the retrospective study design, the effects of iodine exposure could not be determined. An iodine disinfectant is often used during cesarean section and Korean mothers are traditionally encouraged to consume seaweed soup after giving birth. Due to the correlation between maternal iodine consumption and the iodine content of human milk [20], the history of iodine exposure should be investigated. Third, mutations of the gene responsible for synthesis of thyroid hormone were not analyzed. TSH receptor and thyroid peroxidase gene mutations have been reported as causes of subclinical hypothyroidism and transient hypothyroidism [21,22]. Another limitation of this study was that the age at the time of the second screening test significantly differed between SGA infants (26.4 days) and AGA infants (33 days) (P=0.004) due to the retrospective study design. Although the different timing of the second screening may explain the different prevalence of dTSH, 26.4 days is an appropriate age for a second thyroid screening test according to existing guidelines [2].
In conclusion, SGA infants may be at risk of dTSH and clinicians should consider performing a second thyroid screening test in infants at 1 month of age. Although only transient dTSH was observed in this study, early detection and treatment of congenital hypothyroidism are important for improving long-term outcomes. Prospective studies on this topic involving a larger sample of SGA infants are needed.
Notes
Conflicts of interest
No potential conflict of interest relevant to this article was reported.
Funding
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Data availability
The data that support the findings of this study can be provided by the corresponding author upon reasonable request.
Author contribution
Conceptualization: SYP, JHP; Data curation: SK, SYP; Formal analysis: GL, SK, SYP; Methodology: SK; Visualization: SK; Writing - original draft: GL; Writing - review & editing: SK