Near final height in Korean children referred for evaluation of short stature: clinical utility and analytical validity of height prediction methods
Article information
Abstract
Purpose
Predicted adult height (PAH) is often crucial to decision-making about treatment with human growth hormone (GH) or gonadotropin-releasing hormone agonist in children with short stature. This study compares final adult height (FAH) with different methods used to determine PAH and assesses the clinical utility and analytical validity of height prediction for children not treated with GH.
Methods
Clinical findings were retrospectively analyzed, and the heights of 44 children (22 males and 22 females) who visited our clinic between August 2006 and June 2017 and reached near final adult height (NFAH) were evaluated. Children treated with GH were excluded. We compared measured NFAH to PAH using the Bayley-Pinneau (BP), Tanner-Whitehouse Mark 2, and Roche-Wainer-Thissen (RWT) methods.
Results
Pearson correlation between all 3 prediction methods and NFAH showed high positive correlations in males and females (P<0.05). The average difference between PAH and NFAH for the BP method (0.4±3.9 cm) was significantly lower than those for the RWT and TW 2 methods in females (P=0.000, analysis of variance). Furthermore, only PAH by the BP method in females was very close to measured NFAH (paired t-test). A Bland-Altman plot verified that 95% of the differences between the PAH and NFAH exist between limits of agreement (mean±1.96 standard deviation).
Conclusions
The BP method is more useful to predict NFAH in females than other methods. Careful attention is still required when using such tools because PAH can be inaccurate. Therefore, a more accurate FAH prediction model for Korean children is needed.
Introduction
Bone age (BA) determination and prediction of adult height is not only the oldest radiographic procedure but also the most commonly used method for such predictions.
Among prediction tools, the Bayley-Pinneau (BP) method is the most commonly used and familiar method for height prediction. First suggested in 1950 and reworked in 1959, this method is based on BA assessments according to the standards of Greulich and Pyle (GP) [1-3]. Following that, Tanner-Whitehouse (TW) Mark 1 method was introduced in 1975. This was revised to the TW Mark 2 in 1983 and the TW Mark 3 in 2001 [4-6]. Finally, the Roche-Wainer-Thissen (RWT) model was developed in 1975 by Roche and modified in 1993 [7,8], while the BoneXpert model, based on automated BoneXpert BA, was developed in 2009 [9].
Sperlich et al. [10] reported that the difference between the predicted adult height (PAH) using the BP method and observed final height was very small in boys with untreated constitutional growth delay. Maes et al. [11] stated that in short, normal children, the BP method was the most accurate for boys and the TW2 method was the most accurate for girls. Although studies comparing BA assessment using the GP and TW2 methods have been consistently reported [12,13], studies of adult height prediction are sparse in Korea. There is only one report, from 2009, that suggested that the BP method could be the most accurate method for predicting adult height in children with precocious puberty and constitutional growth delay [14].
Therefore, this study evaluated the clinical utility and analytical validity of height prediction testing in Korean children of normal height.
Materials and methods
This study was a retrospective investigation of 2,895 children who presented with subjective complaints of short stature to the Pediatric Endocrinology clinic of Kyung Hee University Hospital at Gangdong between August 2006 and June 2017. First, 5 children with chronic disease and 35 children with endocrine disease were excluded. Seventy-one children were excluded due to interventions with GH or gonadotropin-releasing hormone agonist, and 2,590 children were lost to follow-up. An additional 150 children, who had not achieved final adult height (FAH) at the time of study evaluation, were also excluded. Among 2,895 children, 44 children (22 males and 22 females) who had not been treated with human growth hormone (GH) and reached near final adult height (NFAH) were included in this analysis. Of the 44 children studied, 43 were at normal or normal variants of height above -2 standard deviation score (SDS) for age and sex.
Data gathered from children’s history at the time of initial assessment included age, sex, height, weight, body mass index, and parental heights. Height and weight standard deviation was determined based on the data tables of 2007 Korean Children and Adolescents Growth Standard provided by the Korea Centers for Disease Control & Prevention [15]. Midparental height, PAH, and NFAH SDS was calculated based on the data corresponding to the age of 18.0, which is nearly close to adult height.
BA was rated by an experienced endocrinologist and a radiologist according to the GP and TW2 methods, and PAH at initial assessment was estimated using the BP, RWT, and TW Mark 2 methods [3,5,7]. The BP and RWT methods were based on GP BA and the TW Mark 2 method used TW2 BA. NFAH was measured from June 2016 to June 2017 when height velocity was less than 2 cm/yr, and NFAH was defined for patients with a BA≥16 years for males and BA≥14 years for females.
This research is approved from the Institutional Review Board (IRB) of Kyung Hee University Hospital at Gangdong and written informed consent was exempt from the IRB (KHNMC 2017-07-009-02).
The variables were reported as mean±standard deviation, and a paired t-test was used to compare PAH to NFAH. Oneway analysis of variance (ANOVA) was used to compare differences between PAH and NFAH in males and females separately. Pearson product-moment correlation coefficient was used to examine the relationship between PAH and NFAH. Bland-Altman analyses, proposed in 1983 as an alternative to correlation studies, were used to evaluate the agreement between the observed and PAH and to look for proportional bias [16,17]. Agreement was considered to be statistically significant when P-values were below 0.05. IBM SPSS Statistics ver. 20.0 (IBM Co., Armonk, NY, USA) was used for analysis of data.
Results
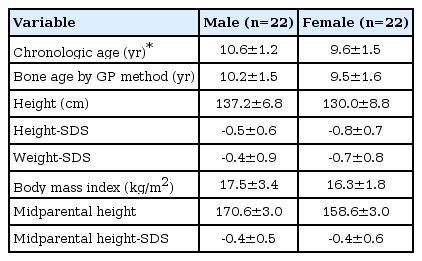
The basal characteristics of study subjects are listed in Table 1. Mean ages of the children were 10.6±1.2 years in males and 9.5±1.5 years in females. Mean heights were 137.2±6.8 cm (-0.5±0.6 SDS; range, -1.64 to 0.53 SDS) in males and 130.0±8.8 cm (-0.8±0.7 SDS; range, -2.14 to 0.3 SDS) in females. Of the 44 children, 43 had heights within normal variation above -2SDS for age and gender. Only one girl had height that was -2.14 SDS. All children showed an insignificant difference between BA and chronological age (CA) (P=0.628).
The mean CAs of the 44 children who had reached NFAH were 16.2±1.2 years in males and 15.2±1.5 years in females. Their mean BAs by GP method were 16.5±0.6 years in males and 15.3±1.1 years in females and their mean BAs by TW2 method were 16.2±0.6 years in males and 15.1±1.1 years in females. The mean NFAHs which were actually observed were 167.8±4.7 cm (-1.0±0.9 SDS) in males and 154.9±5.1 cm (-1.2±1.1 SDS) in females. The PAHs using BP, RWT and TW 2 method were 174.7±4.9 cm, 173.0±3.9 cm and 172.1±4.1 cm in males and were 155.3±3.7 cm, 161.5±3.1 cm, and 159.7±3.5 cm in females (Table 2).

Predicted adult height, final adult height, and their difference according to various prediction methods
The correlation coefficients between the PAH and NFAH according to the different prediction methods are described in Table 3. Pearson correlation between all three prediction methods and final height showed high positive correlations in males and females (P<0.05). The average differences between PAH and NFAH for the BP (6.9±4.2 cm), RWT (5.2±4.1 cm) and TW 2 (4.3±3.7 cm) methods were not significantly different in males (P=0.157, 1-way ANOVA; Table 2). The average difference between PAH and NFAH for the BP method (0.4±3.9 cm) was significantly lower than those for the RWT (6.6±3.6 cm) and TW2 (4.8±4.4 cm) methods in females (P=0.000, 1-way ANOVA). Furthermore, only PAH by the BP method in female was very close to and no different from measured NFAH (paired t-test).
Thus, Bland-Altman analysis was conducted to discern agreement between NFAH and PAH using the BP method, and the difference between PAH using the BP method and NFAH and average height in females is displayed in Fig. 1, which shows considerable agreement between PAH and NFAH. The results of Bland-Altman analysis verified that 95% of the differences between the PAH and NFAH exist between limits of agreement (mean±1.96 SD; 8.0 and -7.1 cm).
Discussion
Several studies have been conducted to validate height prediction models [10,11,14,18-22]. Roemmich et al. [18] reported that the TW2 model gave the most accurate results, followed by the RWT and BP models. Brämswig et al. [19] reported that the RWT method gave very precise results for boys, but no method was superior in estimating adult height for girls. Ostojic [20] reported that that TW2 method was an exact method for PAH in normal-growing athletic boys, while Straetemans et al. [21] found Ranke’s height prediction model for children with idiopathic GH deficiency treated with GH to be accurate.
Despite these varying results, the BP method is the most commonly used and familiar method for height prediction, and many studies including Sperlich et al. [10], Maes et al. [11], and Oh et al. [14] support this model as being effective for adult height prediction. Zachmann et al. [22] also preferred the BP method for children, when growth potential in relation to bone maturation was inherently reduced and could not be corrected by therapy.
In this study, all three prediction methods strongly correlated to NFAHs in males and females (P<0.05). However, only PAH by the BP method in female was very close to and no different from NFAH (paired t-test), and the mean difference between PAH and NFAH for the BP method was significantly lower than those for the RWT and TW2 methods in females (P=0.000, 1-way ANOVA). Additionally, Bland-Altman analysis showed considerable agreement between the means of the differences between NFAH and PAH using the BP method in females. Additionally, Bland-Altman analysis showed considerable agreement between the means of the differences between NFAH and PAH using the BP method in females. Therefore, this study validated that the BP method is more useful than the other methods for predicting FAH in Korean females, which is consistent with previous studies [10,11,14,22].
The strength of this study was that it assessed three height prediction methods (i.e., BP, RWT, and TW2 methods) to compare PAHs with observed FAHs in Korean children. Oh et al. [14] compared PAHs using the BP and TW3 methods in normal children, those with precocious puberty, and those with constitutional growth delay; however, they did not compare PAH and measured adult height and emphasized a need for this type of comparison. Thus, the current research analyzed 44 children of almost normal or normal variants of short stature who exhibited insignificant differences between BA and CA (P=0.628). Since this study group was less heterogeneous than other groups in previous studies, the results of this study can be applied to children with normal and normal variant short stature.
Despite this strength, the present study has some limitations. First, it was a retrospective study, and the size of the final study group was limited. In total, 2,895 children referred for evaluation of short stature, but 5 children with chronic disease, 35 children with endocrine disease were excluded, 71 children were treated with GH, and 2,590 children were lost to follow-up. Although there were an additional 150 children who were not treated, they had not yet achieved FAH and so could not be included in the analysis. The mean intervals between initial and final assessment were 5.5 years for males and 5.6 years for females, which were not long enough for all children being followed up to achieve FAH. It is possible that some children’s ultimate adult height results might be higher. Nonetheless, several other studies on small groups have also yielded valuable results as well as this study [18,23]. An additional limitation is that the BA rating may vary according to the examiner. Finally, we predicted height only once for each of the children, using height prediction methods at the time of the initial visit to the hospital.
In conclusion, PAH using the BP method was closer to the FAH compared to other methods for females and also significantly correlated to the FAH. Thus, the BP method may be more useful for predicting FAH than other methods for females. Although these prediction tools can be helpful in making decisions, careful attention is still required when using such methods because PAH can be inaccurate. In addition, a prospective, long-term study with more cases and a FAH prediction model for Korean children is needed.
Notes
Conflict of interest: No potential conflict of interest relevant to this article was reported.