Impact of targeted education on managing warning and error signals by children and adolescents with type 1 diabetes using the Accu-Chek Combo Insulin Pump System
Article information
Abstract
Purpose
Insulin pumps are widely used in diabetes. They are equipped with safety alarms to alert users. Pump manuals contain alarm codes and how to troubleshoot them. However, these manuals are lengthy and difficult to use, particularly in emergencies. We aim to assess the impact of targeted education on warnings and errors in improving competency to troubleshoot the alarms.
Methods
Twenty-one patients, with a median age of 13, were recruited over a 5-month period. Each patient had 2 study visits. The frequencies and types of alarms were recorded, and patients were given a summary sheet that outlined common alarms encountered and troubleshooting tips. In visit 2, the frequencies and types of alarms were compared to those of visit 1. The patients were asked to fill a questionnaire and to rate the education session given in visit 1, their level of competency in decrypting alarm codes, and their promptness in responding to alarms.
Results
Low cartridge (W1), low battery (W2), and bolus cancelled (W8) were the commonest warnings. The most noted errors were occlusion (E4), power interruption (E8), empty battery (E2), set not primed (E11), and cartridge empty (E1). The numbers of warning and error signals markedly decreased after targeted education (P<0.05). The ability in decrypting warning signals significantly improved (P=0.02), and the frequency of response to pump alarms significantly increased (P=0.001).
Conclusions
Certain warnings and errors are more common than others in insulin pumps. Targeted education is useful in improving competency and response of patients in managing pump alarms.
Introduction
Insulin pump therapy mimics the normal pancreatic function in terms of the insulin profile [1]. Internationally, it has become more popular in the treatment of type 1 diabetes in children and adolescents [2] and has proven to be of benefit in this group of patients [3]. Insulin pumps are equipped with various advanced functions for insulin delivery. However, despite the advances seen in diabetes treatment, the technology has not been as well established as expected, and a specific group of patients has found its application difficult [4]. Accordingly, proper education and understanding are crucial. The lack of adherence to proper pump use is not uncommon, particularly in adolescents, and can be a major factor in the development of short- and long-term complications [5].
Advanced insulin pumps are equipped with safety system monitors that control the pump function. The safety system is accustomed to the pump's "normal-working" state. If a fault occurs within the pump, the normal working state of the pump changes, which triggers an alert. The alert message can be a beep, vibration, or display on the pump screen, indicating the cause of the alert. The Accu-Chek Combo system operates 2 forms of alarms. Warning (W) is an initial stage of an alarm signal that alerts the patient of a situation that may require attention. A warning alert is less serious than an "Error" alarm (E). The latter alerts the patient that the pump has detected a fault that prevents insulin delivery and the pump is switched into a "stop" mode. Various alarms are set at a certain threshold of function. For example, low battery warning (W2) is set when there is 10% battery life left, while low cartridge alerts (W1) are set to go off when a cartridge is at 25% capacity. The pump memory holds up to 30 signals of warnings and errors.
Educating patients on the meanings of alarm codes is necessary. Of particular importance is educating patients about those alerts that may signal a potential interruption in insulin delivery (e.g., an empty battery, an empty cartridge, and occlusion) [6].
The majority of insulin pump manuals have long lists of alarm codes and ways to troubleshoot them. Getting an alarm with an unrecognized code can cause anxiety, and going through a lengthy manual to decrypt a code can be timeconsuming (personal observation). Accordingly, we hypothesize that allocating education sessions targeting pump alarms and providing patients with a written summary of common alerts will increase patients’ competency in dealing with these alarms. In addition, education reduces the frequency of serious alerts that lead to the interruption of insulin delivery.
The aim of the study is to assess the impact of targeted education on reducing the frequency of insulin pump alarms and improving patients' competency in decrypting the warning signals.
Materials and methods
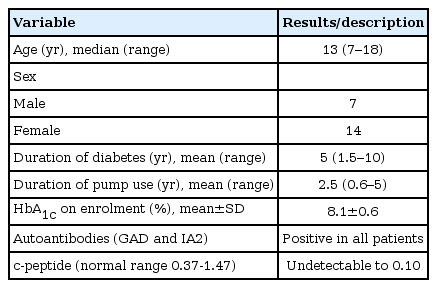
A total of 21 patients were enrolled (14 female patients), and the age range (median) was 7−18 (13) years. All patients had type 1 diabetes mellitus, with a disease duration range (median) of 1.5−10 (5) years. All patients were used the Accu-Check Combo pump, with a duration of use of 0.6−5 (mean, 2.5) years. glycosylated hemoglobin was 8.1±0.6 on enrollment. The enrollment period was between January and May 2015. The patients' characteristics are summarized in Table 1.
The study was approved by the Mafraq Hospital Research and Ethics Committee (approval number: MAF-REC-08/2014_03).
1. Inclusion criteria
• Children and adolescents with type 1 diabetes
• Patients on Accu-Check insulin pump for over 6 months of duration
• Patients who consented to participate in the study
2. Study design
The study consisted of 2 visits to a diabetes clinic 3 months apart. During visit 2, patients were asked to fill out the study questionnaire. The enrollment period was 5 months.
1) Visit 1
During visit 1, patients coming to the clinic for follow-up appointments and who fulfilled the inclusion criteria were approached to participate in the study. The patients were informed about the study by the study team. Those who agreed to enroll in the study gave written consent for their participation. A list of the last 30 errors and warnings encountered were recorded from the patients’ meters. The number constituted the frequency of the pump signals of alarms prior to the targeted education.
The patients attended an education session specifically related to the alarm signaling system. The sessions were administered by an insulin pump certified study team. Warning and error signals stored by the pump were assessed in terms of type and frequency and discussed with patients. Advice on how to manage those signals was discussed verbally, and a summarized manual of signal description was given.
2) Visit 2
During visit 2, the last 30 errors/warnings stored in the meters were recorded. The numbers and types of alarms were compared with those of visit 1. Error and warning signals from visits 1 and 2 were recorded in preparation for the data analysis. The study team explained the questionnaire and highlighted various symbols and their meanings for the enrolled patients.
3. Education method
A team consisting of a diabetes educator, psychologist, and pediatric endocrinologist wrote a protocol targeted to educate patients about pump signal alarms and tips to manage them. The patients and parents/guardians were seen jointly by the team. Various symbols of errors and warnings were explained, and those encountered by each patient were discussed with the individuals. Tips on how to troubleshoot the alarms were given verbally and in writing.
4. Study questionnaire
The questionnaire consisted of 4 questions:
1) Question 1: Ability to decrypt alarm signals
This question relates to the patients' assessments of their ability to understand the warning and error codes and their ability to decrypt the signals. The question was designed utilizing a scale represented by a number from 0 to 100 in 20 increments. The higher the number, the higher the positivity of the answer. In addition to the numerical scale, symbols were used for rating, with facial expressions or bars that the patient could click on. The question was divided into subquestions (a and b) to denote the responses before and after the education assessment.
2) Question 2: Frequency of response to alarm signals
In this question, the patients were asked about the frequency of response to the warning and errors messages. It was designed using a scale of percentage and a facial expression scale as in question 1. The higher the percentage, the higher the promptness and frequency of response to the alarms. In addition, the numerical scale was linked to an ascending order of wording: never, very rarely, often, frequently, most of the time, and always. Question 2 consisted of 2 parts (a and b) to denote the responses before and after the education assessment.
3) Question 3: Subjective assessment of competency in responding to alarm signals
In this question, the patients were asked to assess the impact of the education session on their competency in responding to warnings and errors. Patients indicated their assessment by choosing a number on a scale between 0 and 100. The higher the scale number, the higher the subjective assessment of the impact.
4) Question 4: Method used for troubleshooting alarm signals
In this question, the patients were asked about the method used for seeking help for solving the warning and error signal. The options given were as follows: ask parents, contact diabetes educator, look at the summarized manual given in visit 1, or ignore the signal.
5. Statistical analysis
Paired t-test was used to analyze the change between the samples in the 2 visits. Difference was considered significant if P-value is <0.05. Data analyses were conducted using IBM SPSS Statistics ver. 20.0 (IBM Co., Armonk, NY, USA).
Results
1. Types of warnings and errors encountered during the study period
During the study period, 337 warnings were detected in pumps of all patients. The majority of the warnings were W1 (cartridge low), W8 (bolus cancelled), and W2 (battery low), with a percentage of occurrence of 40%, 31%, and 29%, respectively. A small number of the other noted warnings were related to the temporary basal rate. These were W6 (temporary basal cancelled) and W7 (temporary basal interrupted) (Fig. 1A). Of the 5 main types, 205 errors were found. E4 (occlusion) was the most common error encountered, with a percentage of 46%, followed by E8 (power interruption, which was seen in 18% of the errors. E2 (battery empty), E11 (set not primed), and E1 (cartridge empty) constituted 13%, 10%, and 8% of the errors, respectively. Other less frequent errors consisted of E7 (electric error), E10 (cartridge error), and E12 (data interrupted). These errors constituted the remaining 5% of the errors encountered (Fig. 1B).

(A) Total warnings encountered throughout the study per frequency of occurrence. W1, low cartridge; W8, bolus cancelled; W2, low battery. (B) Total errors encountered by patients in terms of frequency of occurrence. E4, occlusion; E8, power interruption; E2, empty battery; E11, set not primed; E1, empty cartridge.
2. Comparison of frequency of warnings and errors in visits 1 and 2
The number of the 3 main warnings encountered in visit 1 dropped markedly from 213 to 122. The reduction was statistically significant with a P-value <0.001 using a paired t-test. A detailed analysis of the different warning signals showed that W1 dropped from 86 to 39 (P<0.001), W8 from 67 to 39 (P=0.02), and W2 from 71 to 37 (P=0.02) (Fig. 2A). Similarly, a significant reduction in error frequency occurred in visit 2, with the total number of errors dropping from 148 to 57 (P=0.04 using a paired t-test). E4 frequency dropped from 72 to 22 (P<0.001), E8 from 22 to 16 (P=0.04), E2 from 20 to 7 (P=0.02), E11 from 15 to 5 (P=0.02), and E1 from 13 to 3 (P=0.02) (Fig. 2B).
3. Comparison of the ability to decrypt alarm signals and the frequency of response to alarm signals before and after the education visit (Q1a & Q1b, Q2a & Q2b)
The scoring rate of the subjective scale representing the ability to decrypt warning signals (Q1) significantly increased from a mean score of 42 in Q1a to 88 in Q1b (P=0.02). Similarly, the mean score representing the frequency of response to alarms also increased significantly from a mean of 58 in Q2a to 96 in Q2b (P=0.001) (Fig. 3).
4. Subjective assessment of competency in responding to alarm signals following the targeted education session
The mean rating score of the impact of the education session on improving competency in managing the alarm signal was 92% on a scale between 0 and 100.
5. Method used for troubleshooting alarm signals after visit 1
The majority of patients (71%) used the summary manual handed to them in visit 1 in responding and troubleshooting the warning and error alarms. Of the total, 24% asked their parents for help and 5% called the on-call diabetes educator. None of the participants responded with the answer "ignore the warning."
Discussion
Insulin pump therapy has become a popular method for insulin delivery in young people with diabetes [2,3]. However, this therapy involves mastering many functions that some families find difficult [4]. Adapting a multidisciplinary approach, intensifying education, and establishing close follow-up can result in alleviating these difficulties [7]. In our study, targeted education enabled them to troubleshoot the warnings and errors they faced. An analysis of the impact of the education program showed a marked reduction in alarm signals and empowerment of the patients to self-manage pump errors and warnings.
In our studied group, we found 3 commonly encountered warnings and 5 errors. Focusing the training on the commonly seen alarm signals improved patients' competence in using the pump and reduced the frequency of occurrence of both warnings and errors. Low cartridge (W1) was the most common warning encountered by patients. Understanding the reasons leading to an alarm made patients more vigilant in terms of the amount of insulin they needed in each cartridge/set, and it also improved promptness in changing the set at the right time. This resulted in a reduction of the E1 (cartridge empty) sign from 13 to 3 episodes during the study period for all patients (Fig. 2B).
In a typical usage pattern of 50 units/day of U100 insulin and an operating temp of 22℃±3℃, the battery life is approximately 4 weeks for the alkaline and 1 week for the rechargeable batteries. With the warning W2 (battery low), patients paid more attention to the battery life and managed to change the battery in time based on their previous experience, which resulted in reducing the frequency of E2 (battery empty) by a factor of 3 (Fig. 2A).
W8 (bolus cancelled) was a common warning encountered. Some patients cancelled bolus intentionally when they changed their mind about eating or when they did not finish the amount of carbohydrate entered. This was more commonly seen in those using square or combo bolus. Others may have cancelled their bolus when they saw a quick reduction in their blood glucose. In visit 2, this warning was reduced from 67 to 39 episodes.
Delaying tube change beyond that has been documented to cause glucose deterioration and possible occlusion [8]. While occlusion in a set before 72 hours of insertion is uncommon, the risk increases following the 3rd day [9]. Many patients delay changing the sets up to 7 days, which predisposes them to occlusion [10]. The delay in changing the sets could be due to economic reasons, forgetfulness, or deliberate omission.
Occlusion error is an important alarm signal, as it alerts the pump to stop insulin delivery. Technical failures leading to unexpected diabetes ketoacidosis are nowadays rare compared to the early years of pump therapy [11]. However, proper education on how to avoid this complication remains crucial. It is reported that up to 30% of patients with type 1 diabetes on pump therapy experienced an occlusion alarm during a 13-week study [12]. In addition, it is known that interrupting insulin flow due to blockage results in an increase of blood glucose by 1 mg/min, and this rise continues for 3 hours after replacement of the infusion set [13]. Gibney et al. [14] suggested using side infusion pores (flow smart) to reduce the chance of insulin delivery interruption due to occlusion. The frequency of occlusion alarms could be explained by excessive activity by those in the children's age group or delays in changing the pump tubing. In our region, humidity is high, and excessive sweat and rubbing on the insertion site can lead to occlusion. Various tips were given during the education session to prevent occlusion. These included changing the infusion set every 2 to 3 days; inserting the set in a fresh, clean site, which has no lipohypertrophy; and avoiding inserting the set in a pressure area that might lead to blockage of insulin flow. E2 error was dramatically reduced from 72 to 22 episodes in visit 2, indicating that patients took account of the measures discussed to prevent occlusion (Fig. 2B).
Priming the infusion set is an important step in changing the set that can be overlooked (personal observation). The presence of air in the subcutaneous needle results in the blockage of insulin flow and obstruction. The patients reduced the occurrence of this error from 15 to 5 episodes in visit 2 after pointing it out as a common error in visit 1. Switching between the functional (run) and nonfunctional (stop) modes of the pump is an important step for patients to understand. Changing the pump battery, for example, needs to be done when the mode is in "stop" mode. Error E8 (power interruption) was commonly observed in the study’s first visit because many patients had changed their batteries without switching the pumps into the “stop” mode, leading to this error. A reduction was seen in the frequency of this error in visit 2 after the education session (Fig. 2B).
The limitations of our study include the small sample size, short duration of follow-up, and lack of an analyzing the effect on glycemic control. Larger studies to investigate further impacts of targeted education are essential.
In conclusion, our study showed that targeted education towards managing pump alarm signals is effective in reducing their frequency. Warnings and errors are common with insulin pump users, and certain alerts are more common than others. Hence, targeted education on those commonly encountered alerts is beneficial. The verbal and written instructions on alert troubleshooting were highly rated by patients and resulted in marked reductions of warnings and errors.
Notes
Conflict of interest: No potential conflict of interest relevant to this article was reported.
Acknowledgements
We thank Mrs. Suha Mrdash for her invaluable input in training the study team on various technical issues relating to the pump system.