A 3-year-old girl with Graves' disease with literature review
Article information
Abstract
Graves' disease, the main cause of hyperthyroidism in the pediatric age group, is very rare in children younger than 4 years old but can seriously interfere with growth and development if not recognized and treated. Here we report a case of a 3-year-old girl with Graves' disease who presented with goiter, exophthalmos, heat intolerance, and hyperactivity. At her first visit, her serum concentrations of triiodothyronine (T3) and free thyroxine (free T4) were normal, whereas that of thyroid-stimulating hormone (TSH) was decreased. Antimicrosomal antibody was 7,053.94 IU/mL, and TSH-binding inhibitory immunoglobulin was 31.62%. A thyroid scan showed diffuse enlargement with markedly increased uptake of both thyroid glands. Although T3 and free T4 levels were initially normal, she developed hyperthyroidism 3 months later. She was finally diagnosed with Graves' disease and treated with methimazole for 6 months. This is the first report of Graves' disease in children younger than 4 years old in Korea.
Introduction
Hyperthyroidism is uncommon in the pediatric age range and particularly rare in young children. The incidence of hyperthyroidism is 8 cases per 1,000,000 individuals aged 0-15 years per year as reported in the Danish population, and the lowest incidence 1 per 1,000,000 was found in children younger than 4 years1). Graves' disease is the most common cause (95%) of hyperthyroidism, an autoimmune disorder resulting from thyrotropin receptor stimulation by autoantibodies2).
Thyroid hormones play an important role in development of the central nervous system and growth in young children. Hyperthyroidism at that time, if not recognized and treated, can seriously interfere with growth and development, result in irreversible brain damage due to craniosynostosis, failure to thrive, behavior disturbances, and speech impairment, particularly during the first 2 years of life3,4,5,6). Thus, to prevent these complications, early detection and high suspicion of Graves' disease are very important; prompt and proper treatment is also required. We report a case of a 3-year-old girl with Graves' disease who presented with goiter and exophthalmos.
Case report
The patient presented to Presbyterian Medical Center in Jeonju at the age of 3 years and 10 months with a goiter that had progressively enlarged over the previous year. Her parents described her as having excessive sweating, heat intolerance, and hyperactivity. Before she visited our clinic, her medical history was unremarkable. The mother's pregnancy and delivery were uncomplicated. The patient was born at full term with a birth weight of 3,500 g as the first child of the family. There was no family history of thyroid or other autoimmune disease and her mother's thyroid function test was normal.
On physical examination, her vital signs were normal, and no signs of seizures, tremor, or psychomotor abnormalities. Her milestones of motor and mental development had been normal and her height was 106 cm (90th percentile) and weight was 19 kg (90th percentile). Bilateral exophthalmos were observed, while the thyroid was diffusely enlarged to World Health Organization grade 1B and had a soft texture on palpation but no detectable nodules (Fig. 1). No hepatomegaly, splenomegaly, or abnormalities of the chest or abdomen were found.

(A) A 3-year-old girl with Graves' disease. (A-C) Clinical features include a goiter and exophthalmos.
Laboratory studies revealed a normal hemoglobin concentration of 14.6 g/dL, hematocrit of 42.6%, a normal leukocyte count of 7,000/mm3, platelet of 406,000/mm3 and a normal aspartate aminotransferase level of 28 IU/L, alanine aminotransferase of 15 IU/L. On radiologic examination, her bone age was 4.3 years by the Greulich-Pyle method.
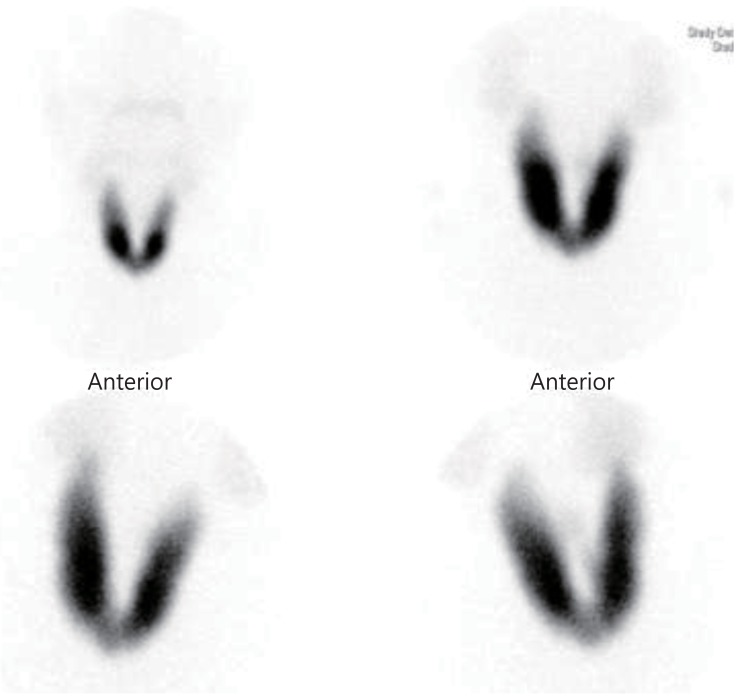
At the first visit, her thyroid-stimulating hormone level (TSH) was 0.03 µIU/mL (normal range, 0.5-4.8 µIU/mL), triiodothyronine (T3) was 1.69 ng/mL (1.19-2.18 ng/mL), and free thyroxine (free T4) was 1.15 ng/dL (0.8-2.2 ng/dL). However, on a follow-up examination, she developed hyperthyroidism with increased values of T3 (2.31 ng/mL) and free T4 (2.25 ng/dL). Antimicrosomal antibody (AMA) was 7.053.94 IU/mL (0-60 IU/mL), TSH-binding inhibitory immunoglobulin (TBII) was 31.62% (positive level>15%). A thyroid scan revealed diffuse enlargement with markedly increased uptake of both thyroid glands (Fig. 2). She was subsequently diagnosed with Graves' disease.
She was treated with methimazole (MMI) in a initial dose of 5 mg twice a day (0.5 mg/kg/day), but other drugs such as β-blockers were not added because she had no palpitation or other thyrotoxic symptoms. Transient hypothyroidism occurred shortly after the therapy was started, but the thyroid function began to recover after a dose reduction. The changes in titers of thyroid function test and TBII and AMA were shown as Table 1. She remains under outpatient follow-up observation (6 months) with MMI in a dose of 1.66 mg once a day (0.08 mg/kg/day), and signs of improvement in the exophthalmos and goiter are evident.
Discussion
Robert Graves first identified the clinical syndrome of goiter, palpitations, and exophthalmos in 1835. Graves' disease is rare in children but is responsible for the vast majority of hyperthyroidism cases in children and adolescents. The incidence of hyperthyroidism is 8 cases per 1,000,000 individuals aged 0-15 years per year as reported in the Danish population, and the lowest incidence of 1 per 1,000,000 was found in children younger than 4 years (excluding those transient hyperthyroid states observed in the neonatal period), and girls are affected four to five times more frequently than boys, although no gender difference is noted in patients younger than 4 years of age1).
There are several reports abroad of Graves' disease in children younger than 4 years6,7,8,9,10,11,12,13), but no such case has yet been reported in Korea. We report this child because of the rarity, the remarkable ophthalmopathy. To sum up a literature review of currently available reports, Segni et al.6), in their report of three cases in girls less than 4 years of age in Italy, presented 12 cases of early childhood Graves' disease to that point, while Rahman et al.7) reported a case of a 3-year-old girl treated with radioactive iodine for medical treatment-induced complications. Coca Perez et al.8) reported four patients less than 6 years old in Spain, two of whom were 4 years or younger, and Karremann et al.10) reported a German case of Graves' disease in a 13-month-old infant suffering from Angelman syndrome. A summary of several cases previously described in the literature, compared to our case is shown in Table 2.
The optimal treatment for Graves' disease in children remains under debate. Current treatment options include antithyroid drugs (ATD), sub- or near-total thyroidectomy, and radioactive iodine. There is no specific cure for the disease and each therapeutic option has associated complications. ATD therapy is usually recommended as the initial treatment for hyperthyroidism in children and adolescents. The most commonly used ATD are carbimazole, its active metabolite MMI, and propylthiouracil (PTU). Avoidance of the use of PTU was recently recommended because of the high risk of PTU-induced hepatitis14). Because MMI has a longer half-life and is effective as a single daily dose, it is particularly helpful in younger children. The frequency of side effects may be dose-related and that of severe side effects is very low in patients receiving carbimazole or MMI at a dose of less than 10 mg/day. The initial starting dose of MMI is 0.5-1 mg/kg/day, with a maximal dose of 30 mg per day. After 2-4 weeks, when thyroid hormone secretion is effectively blocked and thyroid hormone levels have normalized, the initial dose is gradually reduced by 30%-50%. No additional benefit accrues from the maintenance of a high dose of ATD. Additional treatment with β-blockers (except in patients with asthma or cardiac failure) during the first 2 weeks of management may help to reduce the patient's symptoms. This treatment can be given orally twice daily, at a dose of 2 mg/kg/day, and stopped when the patient becomes euthyroid15).
However, medical therapy has potentially serious complications such as agranulocytosis, neutropenia, and drug-induced hepatitis, and young patients usually relapse when treatment is stopped16). Indications for radical treatment in children include ATD toxicity, relapse after an appropriate course of drug treatment, and a lack of compliance on the part of the patient or the parents15). In reports we have seen6,7,8,9,10,11,12,13), all the patients were treated with ATD initially. There was one case report of successful radioiodine treatment in a 3-year-old child with Graves' disease following ATD-induced neutropenia7).
According to the studies on the relationship between age and remission of Graves' disease, prepubertal pediatric patients tend to have an atypical presentation and more severe course, have prolonged treatment durations in inverse proportion to age, be more likely to experience medical treatment failure, and have low remission rates17,18). A remission of Graves' disease on ATD therapy is linked to the restoration of euthyroidism rather than the immunosuppressive effects of the drugs. Hyperthyroidism itself has been shown to worsen the autoimmune aberration, and autoimmunity leads to the generation of more TSH receptor antibody (TRAb) and worsening of hyperthyroidism. Once this cycle is broken by ATD treatment rendering the patient euthyroid or by surgery, the patient may experience gradual remission of the disease15). More prolonged use of ATD (at least 2-4 years) in children than in adults may be required to achieve remission. Compliance is therefore an important issue in the management of these children and should be improved by educational strategies19).
These results are consistent with the generally acknowledged confirmation, as in the current case, that Graves' disease is more difficult to treat in patients less than 4 years old. Thus, considering their adverse reactions to ATD, overall low remission rate, and long remission periods, definitive treatment should be discussed earlier in young children and other therapeutic options discussed with the family.
In conclusion, pediatricians should be aware of the possibility of permanent brain damage due to craniosynostosis, failure to thrive, and neuropsychological deficits in young children with hyperthyroidism, and if Graves' disease is clinically suspected in pediatric patients, special attention should be paid to their ages. The younger the patients are, the closer monitoring is required. Against this background, we reported here a case of Graves' disease that occurred in a 3-year-old girl with a related literature review.
Notes
No potential conflict of interest relevant to this article was reported.