|
 |
- Search
| Ann Pediatr Endocrinol Metab > Volume 20(2); 2015 > Article |
|
Abstract
Vitamin D deficient rickets is generally known to occur in breast fed infants. And excessive phosphate ingestion is a main cause of late onset hypocalcemia in formula fed infants. Here we introduce 45-day-old formula fed hypocalcemic twins with recurrent seizure attacks. They were diagnosed as having both of vitamin D deficient rickets and hyperphosphatemia. Radiologic findings indicated mild rickets and the twins were treated with calcium and alfacalcidol. After 3-5 months of oral supplementation, medication was discontinued in both twins. They showed normal growth and calcium, phosphorus, and vitamin D levels during the 6-month follow-up period. Twins can be at risk for hypocalcemia because of their high risk of vitamin D deficiency, low birth weight, and premature birth. Therefore twin pregnant women need ingestion of sufficient vitamin D and calcium.
Hypocalcemia in infants can be life threatening because it can cause seizures, cardiac rhythm disturbance, and even apnea1). Furthermore, musculoskeletal changes can result from persistent hypocalcemia2). Thus, early diagnosis and management of hypocalcemia is very important in infants. Risk factors for hypocalcemia include premature birth, low birth weight, maternal diabetes mellitus, perinatal asphyxia, and poor intake of vitamin D. Twins may be at risk for hypocalcemia because of their high risk for vitamin D deficiency, low birth weight, and premature birth1,2). Here we introduce 45-day-old twins with recurrent hypocalcemic seizures due to vitamin D deficiency and hyperphosphatemia. Although most cases with hypocalcemic seizure due to vitamin D deficiency are breastfed infants3,4), both of the twins reported here were fed with formula only.
The 45-day-old twin boys were admitted to Keimyung University Dongsan Medical Center because of repeated convulsion without fever. The first twin had four times of generalized tonic clonic seizure events with eyeball deviation and loss of consciousness. He had irritability for 2 days. He was born at a birth weight of 2,200 g after 37 weeks and 4 days of gestation (10-25 percentile for gestational age). He was born in April. On admission, his body weight was 3,900 g (below 3 percentile for his age). He was fed with formula only. Family history was unremarkable. His mother didn't ingest vitamin D during pregnancy.
In the laboratory tests of the first twin, serum total calcium was low at 5.8 mg/dL (normal range, 8.8-10.8 mg/dL) and ionized calcium level was also low at 1.64 mEq/L (normal range, 2.2-2.5 mEq/L). Phosphorus was high at 7.9 mg/dL (normal range, 3.8-6.5 mg/dL). Alkaline phosphatase (ALP) was elevated to 4,503 IU/L (normal range, 100-1,000 IU/L) and immunoreactive parathyroid hormone (iPTH) was elevated to 191.87 pg/mL (normal range, 13-54 pg/mL). The level of 25-hydroxyvitamin D3 (25-D) was very low (5.1 ng/mL; normal range, 10-55 ng/mL). The level of 1,25-hydroxyvitamin D3 (1,25-D) was normal (37.41 pg/mL; normal range, 15-72 pg/mL). Calcitonin was in the normal range. His complete blood cell count, other serum electrolytes, glucose, ammonia, magnesium, blood gas analysis, and albumin level was all in the normal range. Direct bilirubin was elevated to 1.98 mg/dL at diagnosis, but normalized spontaneously. The aspartate aminotransferase (AST) and alanine aminotransferase (ALT) were 49 IU/L and 40 IU/L, respectively. The Îł-glutamyl transferase (Îł-GT) was 64 IU/L.
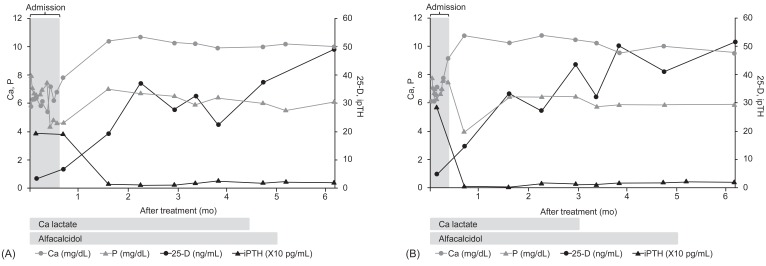
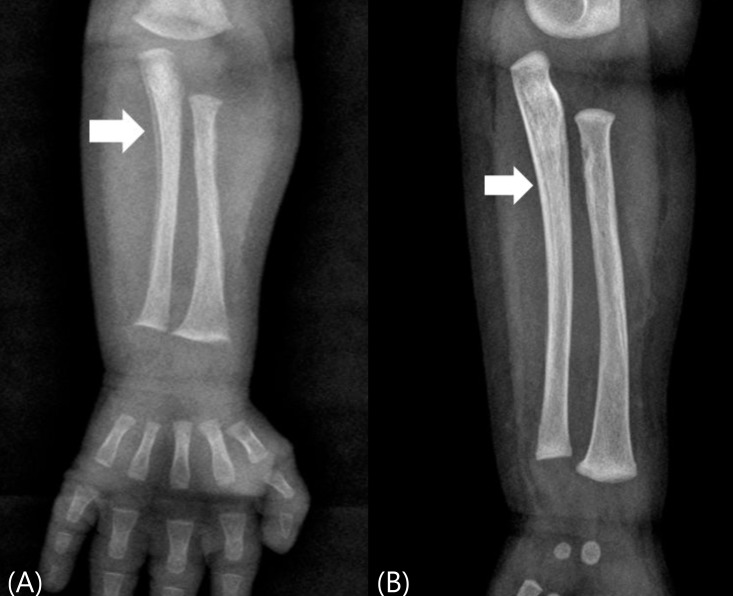
In the radiologic exam, forearm x-ray showed diffuse linear periosteal reaction along the metadiaphyses of his long bones (Fig. 1A). Diffuse osteopenia and vague calvarium, temporal bone was apparent in skull x-ray (Fig. 2). Electroencephalography was normal. He was diagnosed with hypocalcemic seizure due to both vitamin D deficient rickets and hyperphosphatemia based on low calcium, low 25-D, high iPTH, and high phosphorus level.
Phenobarbital was administered to him for 5 days due to recurrent seizure attacks. Intravenous calcium gluconate (200 mg/kg/day) was administered for 4 days during the admission period. Oral calcium lactate (500 mg/kg/day) and alfacalcidol (0.03 Âľg/kg/day) were also administered. On admission day 17, he was discharged without symptoms. We maintained oral calcium lactate and alfacalcidol as same doses for 4.5 months and 5 months, respectively. Thus the doses per weight were tapered spontaneously as his body weight increased. The overall progress of laboratory test results and oral medication period of the first twin are shown in Fig. 3A. After 4 months treatment, when he was 5 months old, the follow-up forearm x-ray showed improved with symmetrical linear periosteal reaction (Fig. 1B).
The second twin had two times of generalized tonic clonic seizure events with eyeball deviation and loss of consciousness at the same day. He was born at a body weight of 2,300 g (10-25 percentile for gestational age). His serum total calcium was 6.2 mg/dL and ionized calcium was 1.77 mmol/L. Phosphorus and iPTH were respectively 7.8 mg/dL and 287.61 pg/mL. ALP was elevated to 3,907 IU/L. The level of 25-D was very low (3.6 ng/mL) and 1,25-D was slightly decreased (14.9 pg/mL). Direct bilirubin was elevated to 3.77 mg/dL at diagnosis, and decreased spontaneously. The AST, ALT, and Îł -GT were 48 IU/L, 29 IU/L and I85 U/L, respectively. The second twin's forearm x-ray and skull x-ray also showed radiologic finding of mild rickets.
Intravenous calcium gluconate was administered to the second twin 2 times during the admission period. Admission period was 11 days. The second twin was managed with 3 months of oral calcium lactate and 5 months of oral alfacalcidol. The overall progress of laboratory test results and oral medication period of the second twin are shown in Fig. 3B. After discontinuation of calcium lactate and alfacalcidol, the twin infants have been followed up for 6 months without additional seizure attacks.
Hypocalcemia is diagnosed when total serum calcium is below 7 mg/dL or ionized calcium is below 1 mmol/L. Neonatal hypocalcemia is categorized into 'early' and 'late' neonatal hypocalcemia according to age. Early neonatal hypocalcemia can develop within 2-4 days after birth. Physiologic decreased calcium levels develop within 1-2 days after birth. If this physiologic hypocalcemia is exaggerated, early neonatal hypocalcemia develops. Late neonatal hypocalcemia can develop within the 1st week to the 6th week after birth. The cause can be transient parathyroid hormone resistance, intake of formula high in phosphorus, DiGeorge syndrome, maternal vitamin D deficiency, hypomagnesemia, malabsorption, or metabolic syndrome. Clinically, distinct differentiation of early and late neonatal hypocalcemia is not always clear1,2). Vitamin D deficiency contributed to over 20% of hypocalcemic infants by Song et al.5).
Generally, breastfed infants are known to have a higher risk of vitamin D deficiency-induced hypocalcemic seizure3,4). However, both of the twins we report here were fed with formula only. In these twin infants, 25-D was very low while 1,25-D was normal or slightly decreased. And phosphorus and iPTH level were high. In vitamin D deficient rickets, serum calcium is decreased at first. And, increased activity of 1a-hydrolase increases 1,25-D level, resulting in normal or only slightly decreased 1,25-D despite of very low 25-D level.
We suspect that the infants reported here had low vitamin D due to decreased transplacental transfer from mother. Maternal vitamin D status is very important to decide the infant's vitamin D level and rickets6,7,8). Vitamin D level is known to be lower in twin pregnancy than in single pregnancies9). This is because higher calcium and vitamin D are required to meet the fetal calcium demand in twins. Furthermore, outdoor activity can be decreased in women with twin pregnancy due to concerns about abdominal tension, resulting in decreased sunlight irradiation.
Thus more sufficient vitamin D supplementation is recommended in women pregnant with twin than women pregnant with single baby. By Society of Maternal-Fetal Medicine, 2,000-2500 mg/day of calcium and 1,000 IU/day of vitamin D intake are recommended in women pregnant with twins10). And 400 IU/day of vitamin D has been recommended to all infants by the American Association of Pediatrics11).
Approximately 1,000 mL of formula contain 400 IU of vitamin D. These twin infants reported here took 500-600 mL/day of formula based on their body weight. In other words, if transplacental transfer of vitamin D was insufficient from mother at birth, formula fed infants also can have vitamin D deficiency. In the study of Choi et al.4), 15.4% of formula fed infants had vitamin D deficiency. Further, it seems that hyperphosphatemia caused by formula feeding (45 mg of phosphorus per 100 mL of formula) aggravated hypocalcemia in these twin infants reported here. And parathyroid hormone resistance and low birth weight also contribute to vitamin D deficiency12,13). Twins tend to have resistance to parathyroid hormone because of the higher frequency of low birth weight or preterm birth for twins compared to single pregnancy.
To summarize, several risk factors of twins in this report-decreased transplacental transfer of vitamin D, hyperphosphatemia from formula feeding, and resistance to parathyroid hormone-seems to have caused recurrent hypocalcemic seizures. Being a twin need to be considered as a risk factor for hypocalcemia. Thus twin pregnant women need ingestion of sufficient vitamin D and calcium.
References
1. Thornton MD, Chen L, Langhan ML. Neonatal seizures: soothing a burning topic. Pediatr Emerg Care 2013;29:1107â1110. PMID: 24084610.



2. Thomas TC, Smith JM, White PC, Adhikari S. Transient neonatal hypocalcemia: presentation and outcomes. Pediatrics 2012;129:e1461âe1467. PMID: 22614771.


3. Kang B, Jung SY, Kim SK, Lee JE, Son BK, Kwon YS. Clinical features of seizures related to rickets in breastfed children. J Korean Child Neurol Soc 2012;20:179â187.
4. Choi YJ, Kim MK, Jeong SJ. Vitamin D deficiency in infants aged 1 to 6 months. Korean J Pediatr 2013;56:205â210. PMID: 23741234.



5. Song JY, Shin YL, Yoo HW. Clinical characteristics of symptomatic hypocalcemic infants. J Korean Soc Pediatr Endocrinol 2002;7:95â104.
6. Thandrayen K, Pettifor JM. Maternal vitamin D status: implications for the development of infantile nutritional rickets. Endocrinol Metab Clin North Am 2010;39:303â320. PMID: 20511053.


7. Kim JW, Han HS. Clinical characteristics of nutritional rickets in Korean infants. J Korean Soc Pediatr Endocrinol 2010;15:51â57.
8. Do HJ, Park JS, Seo JH, Lee ES, Park CH, Woo HO, et al. Neonatal late-onset hypocalcemia: is there any relationship with maternal hypovitaminosis D? Pediatr Gastroenterol Hepatol Nutr 2014;17:47â51. PMID: 24749088.



9. Nakayama S, Yasui T, Suto M, Sato M, Kaji T, Uemura H, et al. Differences in bone metabolism between singleton pregnancy and twin pregnancy. Bone 2011;49:513â519. PMID: 21640859.


10. Goodnight W, Newman R. Society of Maternal-Fetal Medicine. Optimal nutrition for improved twin pregnancy outcome. Obstet Gynecol 2009;114:1121â1134. PMID: 20168116.


11. Wagner CL, Greer FR. American Academy of Pediatrics Section on Breastfeeding. American Academy of Pediatrics Committee on Nutrition. Prevention of rickets and vitamin D deficiency in infants, children, and adolescents. Pediatrics 2008;122:1142â1152. PMID: 18977996.


12. Tsang RC, Chen IW, Friedman MA, Chen I. Neonatal parathyroid function: role of gestational age and postnatal age. J Pediatr 1973;83:728â738. PMID: 4795442.


13. Kim YJ. Comparison of the serum vitamin D level between breastfed and formula-fed infants: several factors which can affect serum vitamin D concentration. Korean J Pediatr 2013;56:202â204. PMID: 23741233.



Fig. 1
Radiologic findings of neonate with hypocalcemic seizure due to vitamin D deficient rickets. (A) In forearm x-ray, diffuse bilateral symmetrical linear periosteal reaction along the metadiaphyses of long bones is shown (white arrow). (B) After treatment, the radiologic finding is improved (white arrow).
- TOOLS
-
METRICS

-
- 3 Crossref
- Scopus
- 12,813 View
- 111 Download
- Related articles in APEM