|
 |
- Search
| Ann Pediatr Endocrinol Metab > Volume 27(4); 2022 > Article |
|
See commentary "Commentary on “Remission in pediatric Graves’ disease treated with antithyroid drug and the risk factors associated with relapse”" in Volume 27 on page 245.
Abstract
Purpose
To evaluate the characteristics and frequency of remission in pediatric patients with Graves’ disease (GD) treated with antithyroid drug (ATD) and to identify factors that may be associated with relapse.
Methods
Medical records of patients younger than 19 years who presented to the Department of Pediatrics of Queen Elizabeth Hospital Hong Kong with newly diagnosed GD from 1st January 2007 to 31st December 2017 were retrospectively reviewed. Remission was defined as euthyroidism for 12 months or more after discontinuation of ATD treatment and no relapses during the follow-up period. Patients who successfully achieved remission were compared to those who suffered relapse. Factors that may predict occurrence of relapse after ATD treatments were studied, and their odds ratios (ORs) were calculated.
Results
A total of 101 patients was included in this study. Eighty-one patients completed one course of ATD. Eighteen patients (17.8%) successfully achieved remission, and 58 patients (57.4%) experienced relapse after discontinuation of ATD. The remission group received a significantly longer course of ATD therapy than the relapse group (median, 28 months; interquartile range [IQR], 18–48 months in remission group vs. median, 21 months; IQR, 17–26; p=0.024). The OR for relapse was 0.971 (95% confidence interval [CI], 0.946–0.997) in univariate analysis and remained significant after adjustments in the multivariate regression model (OR, 0.961; 95% CI, 0.933–0.989; p=0.008).
· The remission rate of pediatric Graves' disease after the first course of antithyroid drug treatment is low.
· Despite a low remission rate, antithyroid drug is still recommended as the first line treatment for pediatric Graves' disease.
· A longer antithyroid drug treatment course is associated with a higher chance of remission in this population.
Graves' disease (GD) causes more than 95% of thyrotoxicosis cases in children [1]. GD is an autoimmune disease caused by an increased level of thyroid stimulating hormone receptor antibodies, which stimulate the thyroid gland to produce excess hormones. The exact mechanism by which individuals produce these autoantibodies is unknown. However, the most accepted hypothesis is that GD is the result of complex interactions between genetic predisposition, environmental factors, and immune system function. The increasing incidence of childhood GD is much higher in Hong Kong than in Western countries [2].
There are 3 options for treatment of pediatric GD: antithyroid drugs (ATD), thyroidectomy, or radioactive iodine (RAI) ablation. Given the more invasive and irreversible nature of surgical treatment and concerns over the use of radiation in young children, definitive treatment options are controversial. Therefore, despite a low remission rate, particularly in the pediatric population [3], oral ATDs are recommended as the firstline therapy in various international guidelines [4-6]. However, the optimal treatment for pediatric GD is not clear. Some recent studies advocate a longer course of ATD, as opposed to the usual 2-year approach, in order to achieve a higher remission rate in children[7-15]. However, a prolonged course of medical treatment is accompanied by problems such as compliance issues, especially in adolescents. Therefore, it would be useful to have reliable predictors of remission or relapse at the time of diagnosis to facilitate selection of treatment options for individual cases.
The aim of this study was to evaluate the characteristics and frequency of remission in pediatric GD patients treated with ATD and to identify factors that may be associated with relapse.
Medical records of patients younger than 19 years who presented to the Department of Pediatrics of Queen Elizabeth Hospital Hong Kong with newly diagnosed GD from 1st January 2007 to 31st December 2017 were retrospectively reviewed. Anti-thyroid-stimulating hormone (TSH) receptor antibody (TRAb) tests were not available until recently and were not routinely performed in our hospital. The diagnoses of GD were reviewed and confirmed by presence of clinical and biochemical thyrotoxicosis (elevated free T4 or free T3 with suppressed TSH) and the presence of at least one of the features suggestive of GD. These features include positive TRAb test; presence of ophthalmopathy; suggestive findings from thyroid ultrasound or thyroid scan; and diffuse, nonnodular, and nontender goitre. Neonatal GD, patients with suspicion of autonomously functioning thyroid nodules and patients with thyroid malignancies were excluded.
Demographic data and clinical characteristics at diagnosis were extracted from medical records, including sex, age at diagnosis, ethnicity, pubertal status, body mass index at diagnosis, family history of autoimmune thyroid disease (defined by positive history in first-degree relatives), personal history of other autoimmune diseases, signs and symptoms of thyrotoxicosis, any documented Graves' ophthalmopathy (GO), types and therapeutic doses of ATD prescribed, and prescription of betablockers. Biochemical results at diagnosis, such as serum free thyroxine (fT4) level, serum free tri-iodothyronine (fT3) level, serum TSH level, and presence of TRAb and antithyroid peroxidase antibody level were collected.
Medical notes and laboratory results of subsequent followup visits were also reviewed in order to obtain information on duration of first ATD course, remission or relapse during follow-up, duration of relapses, receipt of definitive treatment (DT), and duration from date of diagnosis to DT. Data collection was performed in December 2021. Remission was defined as euthyroidism for 12 months or more after discontinuation of ATD treatment and absence of any relapse during the followup period [9]. Relapse was defined as elevated fT4 and/or fT3 together with suppressed TSH that required resumption of ATD and/or led to DT.
Descriptive data were expressed as median (interquartile range, IQR) or frequency (percentage). Pearson chi-square test or Fisher exact test was applied for comparison between categorical variables. Continuous variables were compared by t-test or Mann-Whitney U-test depending on normal distribution status. Univariate and multivariate logistic regression analyses were used to identify potential variables associated with relapse. Variables with P<0.2 in univariate analysis were included in multivariate analysis. The results were expressed as odds ratio (OR) with 95% confidence interval (CI). Statistical analysis was performed using IBM SPSS Statistics ver. 23.0 (IBM Co., Armonk, NY, USA). A P-value of <0.05 was considered significant.
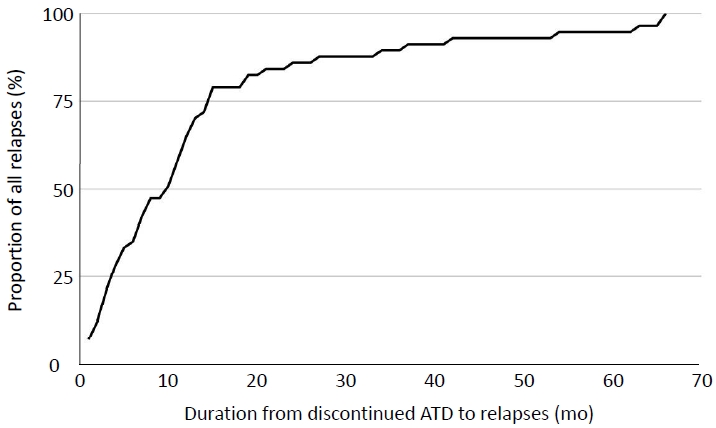
A total of 101 patients, aged four to 18 years at diagnosis, who fulfilled the inclusion criteria was enrolled in the study. Five patients were lost to follow-up during the ATD therapy period, and 8 patients received DT before ATD therapy was tapered. Seven patients received ATD from the time of diagnosis until the time of this study, with a median treatment duration of 61 months (range, 52–132 months). A majority of patients (95%) was prescribed carbimazole (CMZ) after diagnosis. Only 5 patients were started on propylthiouracil (PTU); these patients were diagnosed before the FDA warning of severe hepatic failure risk associated with the use of PTU in 2010. Five patients had skin rash or urticaria after starting on CMZ. Four of these patients required a switch to PTU. No other ATD adverse reactions were observed. Eighty-one patients completed a course of ATD. Eighteen patients (17.8%) successfully achieved remission. Fifty-eight patients (57.4%) experienced relapse after discontinuation of ATD. Five patients were lost to follow-up within 1 year after discontinuation of ATD and did not experience relapse before being lost to follow up. Fig. 1 shows the clinical course of all 101 patients. The baseline demographic and clinical features of the study cohort are given in Table 1. For those who relapsed, the median duration from discontinuation of ATD to relapse was 10 months (IQR, 4-15 months). More than 85% of all relapses occurred within 24 months of discontinuation of ATD, but a few occurred up to 5.5 years later (Fig. 2). Twenty-five patients eventually received DT before or after completion of at least one course of ATD (16 received RAI and 9 underwent surgery). The median duration from diagnosis to DT was 5.6 years (range, 0.8–9.6 years).
The only significant difference between the remission and relapse groups was in follow-up duration and ATD course duration (Table 2). The remission group received a significantly longer ATD course compared to the relapse group (median, 28 months; IQR, 18–48 months in remission group vs. median, 21 months; IQR, 17–26; P=0.024), with an OR of 0.971 (95% CI, 0.946–0.997) for relapse in univariate analysis. After adjusting for other variables with a P-value <0.2 (positive family history for autoimmune thyroiditis and presence of GO) in multivariate analysis, the OR remained significant at 0.961 (95% CI, 0.933– 0.989; P=0.008). All other variables showed no significance in association with relapse (Table 3).
Comparing GD patients among sexes, there were significantly more prepubertal boys than girls (31.3% of boys vs. 10.6% of girls, P=0.012). The median age of diagnosis in boys was slightly younger, 13.3 years (IQR, 11.7-14.6 years), compared to girls 14.5 years (IQR, 11.9-16.4 years); but the difference was not significant (P=0.065). In addition, the group receiving DT (n=25) had a significantly higher fT4 level at presentation (median [IQR]: 73.2 pmol/L [36.0–79.6 pmol/L] vs. 46.7 pmol/L [36.0–79.6 pmol/L]; P=0.036) than those who had never received DT.
The frequency of GD remission after treatment with ATD in this study was 17.8%, which was comparable to that reported in other studies on pediatric GD (range, 11%–49%) [3]. Compared to the reported remission rates in adult studies (range, 39.5%–85%) [9], our finding supported a much lower remission rate in children with GD treated with ATD than in such adults [3,16,17]. Nevertheless, despite a low remission rate with ATD treatment, the other 2 DT options, thyroidectomy and RAI therapy, also have significant limitations. The complication rate for thyroidectomy in children is considerably higher than in adults [18]. For RAI therapy, the total-body radiation dose after 131I therapy varies with age and body size; the absolute dose of 131I results in greater radiation exposure in younger children [19]. There are insufficient studies to draw concrete conclusions regarding future cancer risk related to RAI. Each of the 3 treatment options has its own limitations and shortcomings, and the best treatment modality for pediatric GD patients is unknown.
The optimal duration of ATD treatment in children is also unresolved. ATDs, specifically methimazole or CMZ, the use of which depends upon geographic availability, are currently the recommended first-line treatment for GD. The majority of guidelines suggests that clinicians attempt to reduce or discontinue the dose after 2 years to assess for remission. In cases of failure to achieve remission after 2 years of therapy, DT may be considered instead of continuing ATD. However, these recommendations are largely adopted from adult studies and are guidelines that may not be the most well-suited for the pediatric patient group. Prolonging the duration of ATD treatment in children to increase the success rate of treatment has been advocated in several studies [7-15]. One prospective study published in 2012 by Léger et. al. [7] demonstrated increased remission rates of 20%, 37%, 45%, and 49% after 4, 6, 8, and 10 years of ATD therapy, respectively. Moreover, a randomised trial with a modest sample size of 66 patients published in 2019 showed an almost 3 times higher remission rate in children receiving long-term methimazole (96–120 months) than in those who received short-term therapy (median, 22 months) at 4 years after withdrawal of ATD [10]. Another recent systematic review showed pooled remission rates of 23.7%, 31.0%, 43.7%, and 75% after 1.5–2.5 year, 2.5–5 year, 5–6 year, and 9-year treatment duration, respectively [11]. This concurred with our finding of a significantly longer duration of ATD in the remission group than the relapse group. Despite having a small OR in both univariate and multivariate analyses, significance was achieved even with our small sample size. This suggests one possible therapeutic strategy to improve childhood GD remission rates with a readily available treatment modality. The most recent guideline from the European Thyroid Association for the management of childhood GD in 2022 also recommended a longer phase of initial ATD. This organization recommends that ATD be administered for at least 3 years and potentially for 5 years or more if the likelihood of remission is low [4].
The exact mechanism by which thionamides lead to remission in GD remains uncertain. Thionamides' primary mode of action is to inhibit the oxidation and organification of iodine by inhibiting the thyroid peroxidase enzyme. This prevents iodination of tyrosine residues onto the thyroglobulin molecules. However, the thionamide effect of a decrease in TRAb level has an unknown mechanism. Commonly accepted theories include altering antigen presentation or a direct immunomodulatory action by ATDs [20]. In vitro data suggest that thionamide inhibits thyroid autoantibody production in cultured lymphocytes [20-22]. However, other accumulating evidence suggests otherwise [23,24]. These studies argue that remission of GD during treatment of hyperthyroidism may be linked instead to the restoration of euthyroidism. Hyperthyroidism has been shown to perpetuate, or even to worsen, autoimmunity, leading to greater TRAb production and aggravation of hyperthyroidism [25]. By breaking this vicious cycle through restoration of the patient to a euthyroid state, remission might gradually be achieved [24]. One possibility is that the longer the patient remains euthyroid, the longer their thyroid autoimmunity remains under control, with a higher remission rate and decreased recurrence when ATD administration is discontinued. This could provide the pathophysiological basis for a paradigm shift in managing GD with a longer ATD treatment duration, particularly in children, as their thyrotoxicosis is often more refractory to treatment than adults.
However, long-term ATD has consequences. First, the majority of GD cases involves adolescents in whom compliance is often a major issue. Noncompliance was the reason for the large proportion of patients in our cohort receiving ATD for less than 18 to 24 months. This problem was also addressed by a study in Scotland [26] and should not be overlooked. Second, use of ATD is also associated with several adverse reactions. Minor adverse reactions such as rash, urticaria, arthralgia, and gastrointestinal problems occur in about 5%–25% of cases, while serious complications, such as agranulocytosis, are observed in around 0.2%–0.5% [27]. In our study, we observed minor adverse reactions in 5% of our patients, and none suffered serious complications. Methimazole and CMZ are generally considered to be safe, but continuous monitoring is required throughout the treatment period as side effects may occur well beyond the initial months of treatment [9].
Apart from searching for the optimal duration of ATD therapy, researchers have also tried to identify possible clinical factors at diagnosis that might predict relapses or remissions with ATD. This could help to select patients who are at risk for earlier consideration of DTs. In this study, we were unable to identify any significant factors at diagnosis that were associated with relapse after ATD. Several factors had been suggested to predict a lower occurrence of remission or more relapses after ATD therapy, such as male [12], younger age at diagnosis [8], non-Caucasian ethnicity [8], higher TRAb at diagnosis [8,28,29], higher fT4 level at diagnosis [7,8,12,14], larger goitre size at diagnosis [16], and absence of other autoimmune conditions [7]. Results, however, have not been consistent among studies. Our results showed that patients who received DT had a significantly higher fT4 level at diagnosis compared to those who never received DT. This possibly suggested that patients with more severe thyrotoxicosis at diagnosis require DT. This finding was reported in another study as well [30]. However, caution must be exercised when interpreting this result. The decision-making process for adopting DT in our patients was not standardised and was heavily influenced by patient or parental acceptance of DT.
Given that all existing treatment options are not ideal for managing pediatric GD, novel treatment options should be explored. There were several studies reporting advances in development of therapies that directly inhibit autoantibodies [31-33], but most of these therapies are in early phases of development. More resources should be allocated to this area of research in order to accelerate the development of these treatments and to improve clinical outcomes.
From a more practical point of view, this study showed that, although most relapses occurred within the first 2 years after discontinuing ATD, a small proportion of patients did encounter relapse beyond 2 years (Fig. 2). Consequently, apart from close monitoring clinically and biochemically within 2 years after suspending ATD, GD patients in remission may warrant a longer follow-up duration or self-monitoring education before clinical discharge. Such education is also important when preparing patients for therapeutic tapering or transitioning to adult service.
A major limitation of our study was a small sample size from a single centre. Also, most of our patients did not have TRAb level measured at diagnosis, especially those diagnosed in the earlier years because this test was only made available in our centre recently. TRAb is now routinely measured in all our new cases of thyrotoxicosis and in those preparing for ATD tapering. More data will, therefore, be available for analysis in the future. A few variables of theoretical interests were not included, such as antithyroid peroxidase or antithyroglobulin antibody testing, as assays used to measure antibody titres varied at different time points within our study period and could not be standardised. Other drawbacks include the retrospective nature of this study and the lack of standardised protocol for managing thyrotoxicosis.
To the best of our knowledge, this is one of the small number of Chinese pediatric GD studies identifying factors that may predict relapse after ATD treatment. Non-Caucasian ethnicity is a risk factor for ATD treatment failure, and we appeared to have a higher incidence rate than Western countries [2]. Thus, more local data would be valuable for guiding Asian practice. One advantage of our study is its relatively long follow-up duration compared to other published studies.
Based on our findings, a low remission rate occurs after the first course of ATD in pediatric GD; a longer ATD course was associated with lower risk of relapse. Larger prospective studies are required to define the optimal duration of ATD treatment in children, and more research is essential to explore existing or novel treatment options with better efficacy.
Notes
Funding
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Fig. 1.
Clinical courses of the 101 patients included in this study. ATD, antithyroid drug; DT, definitive treatment.
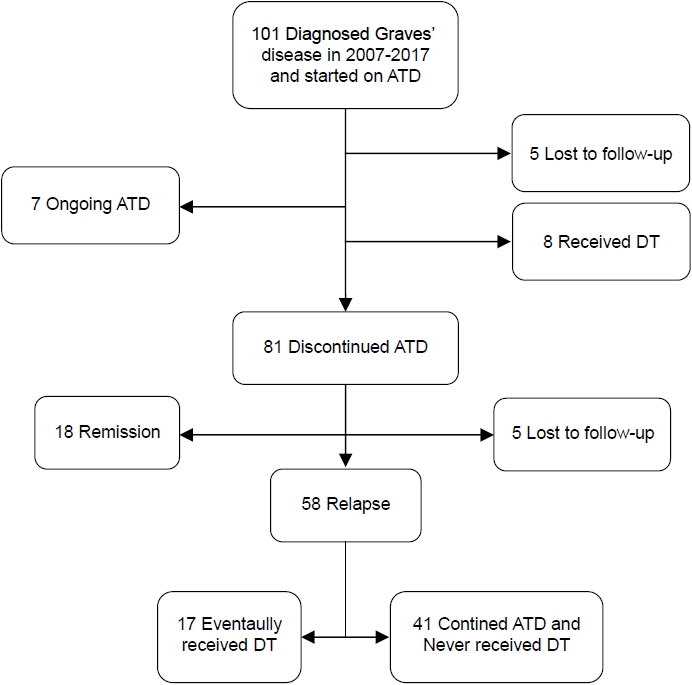
Table 1.
Baseline demographics and clinical features of the study cohort (n=101)
| Variable | Value |
|---|---|
| Age (yr) | 14.11 (11.90-16.02) |
| Male sex | 16 (15.8) |
| BMI (kg/m2) (n=93) | 18.63 (16.83- 20.87) |
| Positive family history* | 36 (35.6) |
| Personal history of autoimmune disease† | 2 (2) |
| Ethnicity | |
| Chinese | 98 (97) |
| Others‡ | 3 (3) |
| Prepubertal (n=99) | 14 (14.1) |
| Presence of GO | 61 (60.4) |
| Follow-up duration (yr) | 7.56 (5.00-10.30) |
| Duration from off ATD to relapse (mo) (n=58) | 10 (11) |
| Received DT | |
| RAI | 16 (15.8) |
| Surgery | 9 (8.9) |
| Duration since diagnosis to DT (yr) (n=25) | |
| RAI | 5.39 (3.85-7.03) |
| Surgery | 7.10 (3.46-8.29) |
| fT4 (pmol/L) (n=96) | 51.45 (49.8) |
| Positive TPOAb titre (n=99) | 90 (90.9) |
| Initial ATD | |
| Carbimazole | 96 (95) |
| Propylthiouracil | 5 (5) |
| Use of beta-blocker (n=96) | 68 (70.8) |
| First ATD course duration§ (mo) (n=81) | 22 (18.00-30.50) |
| Time for fT4 to return normal (day) (n=91) | 45 (25-79) |
Table 2.
Clinical features of patients in remission and relapse group
| Variable | Remission (n=18) | Relapse (n=58) | P-value |
|---|---|---|---|
| Age (yr) | 13.78 (10.31-15.52) | 14.08 (11.74-16.01) | 0.356 |
| Male sex | 3 (16.7) | 9 (15.5) | 1.000 |
| BMI (kg/m2) | 18.12 (15.79-21.77) | 18.39 (16.92-20.18) | 0.529 |
| Positive family history† | 9 (50) | 18 (31) | 0.142 |
| Personal history of autoimmune disease | 0 (0) | 0 (0) | - |
| Chinese ethnicity | 17 (94.4) | 57 (98.3) | 0.420 |
| Prepubertal | 4 (22.2) | 7 (12.1) | 0.278 |
| Presence of GO | 8 (44.4) | 37 (63.8) | 0.145 |
| Follow-up duration (yr) | 6.04 (4.86-9.35) | 8.25 (6.54-10.38) | 0.037 |
| fT4 at diagnosis (pmol/L) | 62.2 (33.4-93.1) | 53.45 (37.50-98.48) | 0.962 |
| Positive TPOAb titre at diagnosis | 17 (100) | 52 (89.7) | 0.327 |
| Use of beta-blocker at diagnosis | 13 (81.3) | 37 (66.1) | 0.359 |
| First ATD course duration (mo) | 28 (18-48) | 21 (17-26) | 0.024 |
| Time for fT4 to return normal (day) | 45 (29-59) | 39.5 (24.25-84.25) | 0.657 |
Table 3.
Odds ratio of individual variables for relapse in patients treated with a course of antithyroid drugs
| Variable |
Unadjusted OR |
Adjusted OR |
||||
|---|---|---|---|---|---|---|
| OR | 95% CI | P-value | OR | 95% CI | P-value | |
| Age (yr) | 1.099 | (0.934–1.294) | 0.254 | - | - | - |
| Male sex | 0.918 | 0.220–3.833 | 0.907 | - | - | - |
| BMI (kg/m2) | 1.055 | 0.879–1.265 | 0.565 | - | - | - |
| Positive family history† | 0.450 | 0.153–1.323 | 0.147 | 0.398 | 0.123–1.286 | 0.124 |
| Non-Chinese ethnicity | 0.298 | 0.018–5.025 | 0.401 | - | - | - |
| Prepubertal | 0.480 | 0.123–1.878 | 0.292 | - | - | - |
| Presence of GO | 2.202 | 0.753–6.439 | 0.149 | 3.308 | 0.962–11.382 | 0.058 |
| fT4 at diagnosis (pmol/L) | 0.998 | 0.978–1.019 | 0.848 | - | - | - |
| Use of beta-blocker at diagnosis | 0.449 | 0.114–1.772 | 0.253 | - | - | - |
| First ATD course duration (mo) | 0.971 | 0.946–0.997 | 0.030 | 0.961 | 0.933–0.989 | 0.008 |
| Time for fT4 to return normal (day) | 1.001 | 0.996–1.005 | 0.784 | - | - | - |
References
2. Wong GW, Cheng PS. Increasing incidence of childhood Graves' disease in Hong Kong: a follow-up study. Clin Endocrinol (Oxf) 2001;54:547–50.



3. Léger J, Carel JC. Management of endocrine disease: arguments for the prolonged use of antithyroid drugs in children with Graves' disease. Eur J Endocrinol 2017;177:R59–67.


4. Mooij CF, Cheetham TD, Verburg FA, Eckstein A, Pearce SH, Léger J, et al. 2022 European Thyroid Association Guideline for the management of pediatric Graves' disease. Eur Thyroid J 2022;11:e210073.


5. Ross DS, Burch HB, Cooper DS, Greenlee MC, Laurberg P, Maia AL, et al. 2016 American Thyroid Association Guidelines for diagnosis and management of hyperthyroidism and other causes of thyrotoxicosis. Thyroid 2016;26:1343–421.


6. Committee on Pharmaceutical Affairs; Japanese Society for Pediatric Endocrinology, and the Pediatric Thyroid Disease Committee; Japan Thyroid Association (Taskforce for the Revision of the Guidelines for the Treatment of Childhood-Onset Graves' Disease); Minamitani K, Sato H, et al. Guidelines for the treatment of childhood-onset Graves' disease in Japan, 2016. Clin Pediatr Endocrinol 2017;26:29–62.



7. Léger J, Gelwane G, Kaguelidou F, Benmerad M, Alberti C, French Childhood Graves' Disease Study Group. Positive impact of long-term antithyroid drug treatment on the outcome of children with Graves' disease: national longterm cohort study. J Clin Endocrinol Metab 2012;97:110–9.


8. Kaguelidou F, Alberti C, Castanet M, Guitteny MA, Czernichow P, Léger J, et al. Predictors of autoimmune hyperthyroidism relapse in children after discontinuation of antithyroid drug treatment. J Clin Endocrinol Metab 2008;93:3817–26.


9. Ohye H, Minagawa A, Noh JY, Mukasa K, Kunii Y, Watanabe N, et al. Antithyroid drug treatment for graves' disease in children: a long-term retrospective study at a single institution. Thyroid 2014;24:200–7.


10. Azizi F, Takyar M, Madreseh E, Amouzegar A. Longterm methimazole therapy in juvenile Graves' disease: a randomized trial. Pediatrics 2019;143:e20183034.



11. van Lieshout JM, Mooij CF, van Trotsenburg ASP, Zwaveling-Soonawala N. Methimazole-induced remission rates in pediatric Graves' disease: a systematic review. Eur J Endocrinol 2021;185:219–29.


12. Bayramoğlu E, Elmaogulları S, Sagsak E, Aycan Z. Evaluation of long-term follow-up and methimazole therapy outcomes of pediatric Graves' disease: a singlecenter experience. J Pediatr Endocrinol Metab 2019;32:341–6.


13. Tunç S, Köprülü Ö, Ortaç H, Nalbantoğlu Ö, Dizdarer C, Demir K, et al. Long-term monitoring of Graves' disease in children and adolescents: a single-center experience. Turk J Med Sci 2019;49:464–71.



14. Song A, Kim SJ, Kim MS, Kim J, Kim I, Bae GY, et al. Long-term antithyroid drug treatment of Graves' disease in children and adolescents: a 20-year single-center experience. Front Endocrinol (Lausanne) 2021;12:687834.



15. Rabon S, Burton AM, White PC. Graves' disease in children: long-term outcomes of medical therapy. Clin Endocrinol (Oxf) 2016;85:632–5.



16. Glaser NS, Styne DM. Predictors of early remission of hyperthyroidism in children. J Clin Endocrinol Metab 1997;82:1719–26.


18. Sosa JA, Tuggle CT, Wang TS, Thomas DC, Boudourakis L, Rivkees S, et al. Clinical and economic outcomes of thyroid and parathyroid surgery in children. J Clin Endocrinol Metab 2008;93:3058–65.



19. Rivkees SA. Controversies in the management of Graves' disease in children. J Endocrinol Invest 2016;39:1247–57.



20. Cheetham T. How to use thionamide anti-thyroid drug in the young- what's new? Thyroid Res 2021;14:18.




21. Weetman AP, McGregor AM, Hall R. Methimazole inhibits thyroid autoantibody production by an action on accessory cells. Clin Immunol Immunopathol 1983;28:39–45.


22. Tötterman TH, Karlsson FA, Bengtsson M, Mendel-Hartvig I. Induction of circulating activated suppressor-like T cells by methimazole therapy for Graves' disease. N Engl J Med 1987;316:15–22.


23. Wenzel KW, Lente JR. Similar effects of thionamide drugs and perchlorate on thyroid-stimulating immunoglobulins in Graves' disease: evidence against an immunosuppressive action of thionamide drugs. J Clin Endocrinol Metab 1984;58:62–9.


24. Laurberg P. Remission of Graves' disease during antithyroid drug therapy. Time to reconsider the mechanism? Eur J Endocrinol 2006;155:783–6.


25. Volpé R. The immunomodulatory effects of anti-thyroid drugs are mediated via actions on thyroid cells, affecting thyrocyte-immunocyte signalling: a review. Curr Pharm Des 2001;7:451–60.


26. Kourime M, McGowan S, Al Towati M, Ahmed SF, Stewart G, Williamson S, et al. Long-term outcome of thyrotoxicosis in childhood and adolescence in the west of Scotland: the case for long-term antithyroid treatment and the importance of initial counselling. Arch Dis Child 2018;103:637–42.


27. Kaguelidou F, Carel JC, Léger J. Graves' disease in childhood: advances in management with antithyroid drug therapy. Horm Res 2009;71:310–7.



28. Gu Y, Liang X, Liu M, Wu D, Li W, Cao B, et al. Clinical features and predictors of remission in children under the age of 7 years with Graves' disease. Pediatr Investig 2020;4:198–203.




29. Gastaldi R, Poggi E, Mussa A, Weber G, Vigone MC, Salerno M, et al. Graves disease in children: thyroid-stimulating hormone receptor antibodies as remission markers. J Pediatr 2014;164:1189. –94. e1.


30. Jevalikar G, Solis J, Zacharin M. Long-term outcomes of pediatric Graves' disease. J Pediatr Endocrinol Metab 2014;27:1131–6.


31. El Fassi D, Banga JP, Gilbert JA, Padoa C, Hegedüs L, Nielsen CH. Treatment of Graves' disease with rituximab specifically reduces the production of thyroid stimulating autoantibodies. Clin Immunol 2009;130:252–8.